Day :
- Heart Diseases | Electrocardiography | Diabetes & Heart | Cardiac Regeneration | Cardiomyopathies | Cardiac Nursing
Location: Amphi Theatre

Chair
Guy Hugues Fontaine
Universite Pierre et Marie Curie & La Salpetriere Hospital, France

Co-Chair
William E Feeman Jr.
Wood County Hospital, USA
Session Introduction
William E Feeman Jr.
Wood County Hospital, USA
Title: Enhanced prediction of the population at risk of atherothrombotic disease
Time : 11:30-11:55

Biography:
William E Feeman Jr is a Physician on staff at Wood County Hospital, and private practice, Bowling Green, Ohio. He is the Founder of Association for the Prevention of Atherothrombotic Disease in Northwest Ohio to facilitate the spread of knowledge about this disease.
Abstract:
Statement of the Problem: To be able to prevent atherothrombotic disease (ATD), one must be able to predict the population at risk of ATD. Many risk predictors have been advocated for such prediction, but none have been universally accepted.
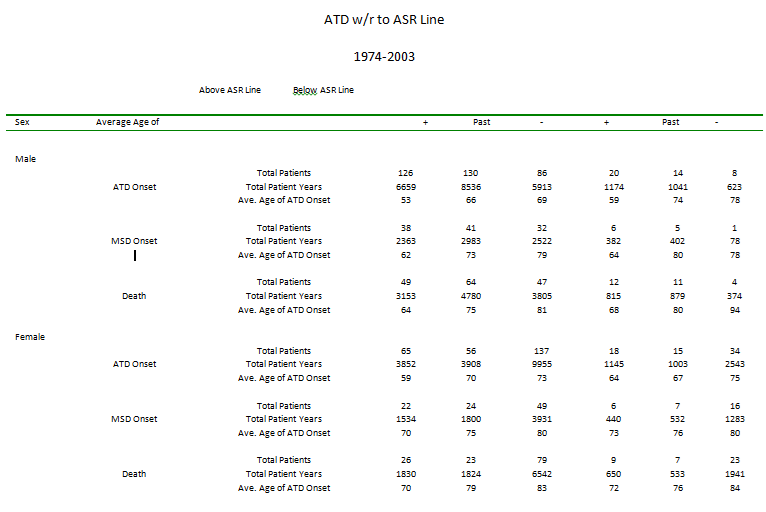
Methodology & Theoretical Orientation: The Framingham Heart Study has demonstrated that the population that develops ATD differs from the population that does not by the severity of certain ATD risk factors and the duration during which those risk factors have been operative. The author has examined his entire ATD population to determine the constellation of ATD risk factors that separates population from the population that did not develop some form of clinical ATD.
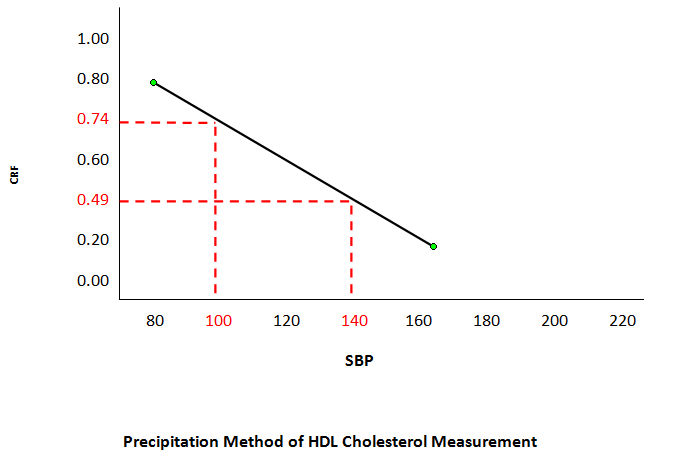
Findings: The population at risk of ATD is characterized by cigarette smoking, dyslipidemia, and (often) hypertension, with some contribution from the very high blood sugar levels of uncontrolled diabetes. These risk factors are not independent, but rather dependent, interacting with one another leading to ATD. Dyslipidemia is defined as a ratio between LDL- and HDL-cholesterol (Cholesterol Retention Fraction, or CRF, defined as [LDL-HDL]/LDL). The predictive tool is a graph with the CRF on the ordinate and systolic blood pressure (SBP) on the abscissa. The graph exhibits a threshold line with CRF-SBP co-ordinates (0.74, 100) and (0.49, 140), above which lie the CRF-SBP of 93% of all the ATD patients in the author’s practice. Further fine-tuning can be done by stratifying the CRF by SBP or by LDL-cholesterol. Any therapy that brings the CRF-SBP plot below the threshold line results in plaque stabilization/regression in a minimum average of 75% of cases.
Conclusions: The population at risk of ATD is predictable and hence, ATD is preventable.
References:
- Feeman Jr., WE, Willliams SE, Buckwald H. The Program on the Surgical Control of the Hyperlipidemias (POSCH) and the Lipid Regulatory Hypothesis. Europeon Medical Journal of Cardiology. 2015; 3 (1): 67-76.
- Feeman Jr. WE. LDL lowering: Evidence for a Plaque Non-Progression Threshold. Int J Cardiovasc Res. 2013; 2: 5.
- Feeman W.E. Jr. Prediction of the Population at Risk of Atherothrombotic Disease. Experimental and Clinical Cardiology. Winter 2004. 9: (4); 235-241.
- Feeman W.E. Jr. Statin Therapy in a 101 Year Old Survivor of Myocardial Infarction-Submitted to European Medical Journal (Cardiology) and under review for publication.
- Feeman W.E. Jr. Concerns About the Use of Non-HDL Cholesterol as a Lipid Predictor.
Issam A Mikati
Northwestern University, USA
Title: The use of strain imaging in detection and management of patients with early cardiomyopathy
Time : 11:55-12:20

Biography:
Issam Mikati completed his Graduation at American University of Beirut Medical School. He completed his Cardiology and Imaging fellowship at Baylor College of Medicine. He is an Associate Director of Echocardiography lab at Northwestern Memorial hospital in Chicago, Illinois. He has published numerous papers in reputed journals and has served as a Reviewer of premier journals.
Abstract:
Cardiomyopathy confers a poor prognosis. Early recognition and intervention is very important to improve outcome. Classic method of assessment of LV systolic dysfunction such as Left Ventricular Ejection Fraction (LVEF) suffer from wide variance that limits their utility in detection of minor changes in systolic function on serial testing. In addition, the changes in LVEF appear late after significant myocardial damage has occurred. This has been shown to affect prognosis of patients. Strain has been shown to be an accurate sensitive marker of LV function with less variance than traditional methods of LV systolic function. It has been shown to drop early in the natural history of many systemic diseases that affect the heart such as diabetic cardiomyopathy. Strain shows great promise in management of cardiomyopathies because of its efficacy in early detection and potentially effects of treatment.
Katriina Aalto-Setala
University of Tampere, Finland
Title: Genetic ventricular arrhythmia: Clinical presentation and disease modeling using iPSC-derived cardiomyocytes
Time : 12:20-12:45

Biography:
Katriina Aalto-Setälä is the Professor of Physiology at School of Medicine, University of Tampere and a Cardiologist at Heart Hospital, Tampere University Hospital, Finland. She works as an invasive Cardiologist and is In-charge of the genetic cardiac outpatient clinic at Heart Hospital. Her research at University of Tampere focuses on Human Genetic Cardiac Diseases such as genetic arrhythmias and atherosclerosis with the help of induced pluripotent stem cell (iPSC) technology. The main aim of the research group is to learn more about the basic pathology of the genetic diseases as well as to test current and new pharmaceutical agents to correct the abnormalities. Her research group in collaboration with researches at Tampere Technical University has also invented new methods to monitor and analyze the maturity and functionality cardiomyocytes.
Abstract:
Background: Genetic cardiac arrhythmias are often severe, but due to their rare nature, no specific treatment exists. Catecholaminergic polymorphic ventricular tachycardia (CPVT) is a severe arrhythmia caused by mutations in the RyR2 gene. This gene is important in regulating Ca2+ release from sarcoplasmic reticulum. The purpose of this study was to create induced pluripotent stem cells (iPSCs) from individuals having CPVT and to study the functional properties of the cardiomyocytes.
Methodology: iPSC lines were derived from six individuals carrying different RyR2 gene mutations. Arrhythmias of cardiomyocytes were analyzed using Ca2+ imaging.
Findings: Patients’ heart rates were increased by stress exercise test and this induced in all of them polymorphic ventricular extra beats. When their cardiomyocytes were treated with adrenaline, similar irregular beating was observed. If the patients were treated with dantrolene, in some individuals all arrhythmias were abolished, but in some, it did not have any effect. As their cardiomyocytes were treated with the same drug, adrenaline-induced arrhythmias were abolished, but only from those cardiomyocytes derived from individuals who also clinically responded to the treatment. However, arrhythmias were not abolished from cardiomyocytes derived from the patients having no response to the medication.
Conclusion & Significance: With this drug, we could demonstrate that all individuals did not respond to this medication the same way even though their clinical phenotype was the same and they had mutations in the same gene. Importantly, iPSC-derived cardiomyocytes demonstrated the very same phenomenon: If the patient responded, also his cardiomyocytes responded, but if the drug did not remove arrhythmias from the patient, they were not abolished from his cardiomyocytes either. This study demonstrate that iPSC-derived cells reproduce the effect observed in the patients and they could be used to tailor medication especially in patients having severe, potentially lethal arrhythmias.
References:
- Aalto-Setälä K, Conklin BR, and Lo, B. Obtaining consent for future research with induced pluripotent cells: Opportunities and challenges. PLoS Biology 7:e42, 2009.
- Lahti AL, Kujala VJ, Pekkanen-Mattila M, Kerkelä E, Chapman H, Koivisto A-P, Hyttinen J, Kontula K, Swan H, Yamanaka S, Conklin B, Silvennoinen O, Aalto-Setälä K. Cardiomyocytes derived by iPS cell technology from a long QT syndrome type 2 patient display the disease phenotype. Disease Models and Mechanisms 2012 Mar;5(2):220-30. doi: 10.1242/dmm.008409. Epub 2011 Nov 3.
- Kujala, K., Paavola, J., Lahti, A., Larsson, K., Pekkanen-Mattila, M., Viitasalo, M., Lahtinen, A.M., Toivonen, L., Kontula, K., Swan, H., Laine, M., Silvennoinen, O., and Aalto-Setälä, K. Cell Model of Catecholaminergic Polymorphic Ventricular Tachycardia Reveals Early and Delayed Afterdepolarizations PLoS ONE 2012;7(9):e44660. Epub Sep 4, 2012.
- Kiviaho AL., Ahola, A., Larsson, K., Kujala K., Pekkanen-Mattila, M., Venäläinen, H., Paavola, K., Hyttinen J. and Aalto-Setälä, K. Distinct electrophysiological and mechanical beating phenotypes of Long QT syndrome type 1 -specific cardiomyocytes carrying different mutations. International Journal of Cardiology, 8:19-31, 2015
- Penttinen, K , Swan H, Vanninen, S, Paavola J, Lahtinen A.M., Kontula, K and Aalto-Setälä K. Demonstration of the Antiarrhythmic Effect of Dantrolene in a Subset of CPVT Patients That is Predicted in iPSC Model PLoS One, Aug 26;10(8):e0135806. doi: 10.1371/journal.pone.0135806. eCollection 2015.
- Penttinen K, Siirtola H, Ávalos-Salguero J, Vainio T, Juhola M, Aalto-Setälä K. A Novel Analysis Software to Detect and Classify Ca2+ Transient Abnormalities in Stem Cell Derived Cardiomyocytes. Plos One, PLoS One. 2015 Aug 26;10(8):e0135806. doi: 10.1371/journal.pone.0135806. eCollection 2015
- Ojala M, Prajapati C, Pölönen R-P, Rajala K, Pekkanen-Mattila M, Larsson K, Aalto-Setälä K Mutation-specific phenotypes in hiPSC-derived cardiomyocytes carrying either myosin-binding protein C or α-tropomyosin for hypertrophic cardiomyopathy. Stem Cells International 2016, ID 1684792.
- Special Session on: "Diastolic stress echocardiography: How and when to perform it"
Location: Amphi Theatre
Session Introduction
Fabiola B Sozzi
University Hospital Policlinico of Milan, Italy
Title: Diastolic stress echocardiography: How and when to perform it
Time : 13:45-14:45

Biography:
Fabiola B Sozzi works as a Staff Cardiologist at University Hospital Policlinico of Milan, Italy. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She has expertise in Echocardiography at Thoraxcenter of Rotterdam (NL), where she defended her PhD thesis on Stress Cardiac Imaging under the supervision of Professor J Roelandt. She is a Visiting Professor at University of Milan where she leads several research projects and teaches at Faculty of Medicine and School of Specialization of Cardiology. She is an Author of 70 papers published in peer-reviewed international journals and Reviewer of several medical international journals.
Abstract:
There is growing evidence that the diastolic stress test can provide important diagnostic findings helpful in the management of patients presenting with dyspnea of an unclear etiology. Many patients present with exertional dyspnea and exercise intolerance, but have normal left ventricular filling pressures at rest. In these patients, it is important to evaluate filling pressure with exercise. Exercise can be performed using a supine bicycle or treadmill protocol. Alternatively dobutamine can be used, though its vasodilator as well as inotrope effect determine a very different hemodynamic response compared to that of exercise. We need to record mitral inflow by pulsed Doppler echocardiography at the level of the mitral tips, mitral annular velocities by spectral Doppler echocardiography, and tricuspid regurgitation jet by continuous-wave Doppler at baseline and after the termination of exercise. Diastolic function parameters can be obtained soon after the assessment of regional wall motion abnormalities, especially when an exercise echocardiogram is performed for the evaluation of dyspnea. In patients with diastolic heart failure, left atrial pressure is increased, leading to an increase in mitral E velocity, whereas annular e’ velocity remains reduced given the limited preload effect on e’. Moreover, an increase in the pulmonary artery systolic pressure can be detected by the increase in peak velocity of the tricuspid regurgitation jet. On the other hand, in the absence of cardiac disease, e’ increases to a similar extent to the increase in mitral E velocity, and the normal E/e’ ratio essentially is unchanged with exercise. The concept of the diastolic stress test was introduced more than 10 years ago. Subsequently, exercise E/e’ ratio was validated against invasive measurements. Importantly, exercise septal E/e’ ratio was an important determinant of exercise capacity, and its decline with age was noted in a large series of patients referred for exercise echocardiography. Furthermore, a recent study showed the incremental prognostic value of exercise E/e’ ratio over clinical variables and exercise wall motion score index. In conclusion, diastolic stress test has an interesting role in patients with heart failure and preserved ejection fraction that present symptoms during activity, normal ejection fraction and inconclusive diastolic function at rest.
- Cardiac Regeneration | Heart Diseases | Diabetes & Heart | Cardiomyopathies | Cardiac Nursing | Electrocardiography
Location: Amphi Theatre

Chair
Guy Hugues Fontaine
Universite Pierre et Marie Curie & La Salpetriere Hospital, France

Co-Chair
William E Feeman Jr.
Wood County Hospital, USA
Session Introduction
Suzanne Tinsley
Louisiana State University Health-Shreveport, USA
Title: Assistive technology utilized for cardiovascular conditioning for patients with spinal cord injury: A case study
Time : 14:45-15:10

Biography:
Suzanne Tinsley received her PT degree at Texas Woman’s University and PhD in Neuropharmacology at Louisiana State University Health Sciences Center. She received her Board Certification in Neurologic Physical Therapy at American Board of Physical Therapy Specialties (ABPTS). She has been a Faculty member at LSU-Health since 1988 and currently holds the position of Associate Professor. She has published a Pharmacology text book for physical therapy education. She has an active clinical research program in the area of Neurological Rehabilitation.
Abstract:
Statement of the Problem: There are between 183,000 and 230,000 people with spinal cord injury (SCI) living in United States, with approximately 11,000 new cases each year. In spite of the advancements in medical and educational interventions, individuals with SCI still face health disparities and a number of challenges in maintaining cardiovascular health compared to the able bodied population. As a result, heart disease (HD) is one of the leading causes of death for patients with chronic SCI. Providing effective interventions to reduce the effects of HD for individuals with SCI is vital.
Purpose: Demonstrate the cardiovascular benefits of ambulation with a hybrid orthotic-functional electrical stimulation system (ARGO-FES) in a patient with paraplegia when performed in a clinical setting. Sample: Single-subject case study involving a patient with paraplegia enrolled in an outpatient rehab program for ambulation.
Method: Participant engaged in an ARGO-FES ambulation program 20 minutes, two times a week for six weeks. The following variables were measured at each session: pre- and post-exercise heart rate (HR) and blood pressures (BP) and distance ambulated. In addition, cholesterol (total, HDL/LDL ratio), and serum triglycerides were measured at baseline and at the end of the six-week intervention.
Findings: Patient demonstrated cardiovascular conditioning with reductions in post-ambulation HR and pulse pressure with an increase in distance ambulated. Triglycerides remained unchanged, LDL cholesterol decreased, and HDL cholesterol increased after six weeks of intervention.
Conclusion: Cardiovascular conditioning with an ARGO-FES system conducted in a clinical setting can reduce cardiovascular risk factors and facilitate health in individuals with chronic SCI.
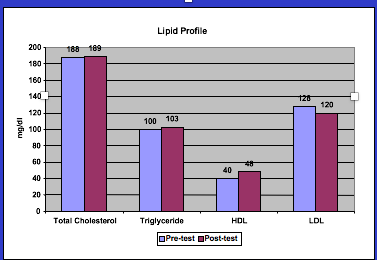
Figure: Pre- and post-exercise training total cholesterol, triglycerides, HDL’s, and LDL’s blood lipid profile.
References:
- Cragg JJ, et al. (2015) Neuropathic pain, depression and cardiovascular disease: A national multicenter study. Neuroepidemiology 44(3):130-137
- Kerstin W, et al. (2006) What promotes physical activity after spinal cord injury? An interview study from a patient perspective. Disability & Rehabilitation 28(8):481-488.
- Bauman WA et al. (1998) The effect of residual neurological deficit on serum lipoproteins in individuals with chronic spinal cord injury. Spinal Cord 36(1):13-17.
- Groah SL, Menter RR. (1998) Long-term cardiac ischemia leading to coronary artery bypass grafting in a tetraplegic patient. Archives of Physical Medicine and Rehabilitation 79(9):1129-1132.
- Solomonow M et al. (1997) Reciprocating gait orthosis powered with electrical muscle stimulation (RGO II). Part II: Medical evaluation of 70 paraplegic patients. Orthopedics 20(5):411-418.
Marie Vazquez Morgan
Louisiana State University Health-Shreveport, USA
Title: Use of a functional electrical stimulation bike to improve cardiovascular risk factors in an individual with spinal cord injury in a clinical setting
Time : 15:10-15:35

Biography:
Morgan earned a BS in Physical Therapy and her academic doctorate in Health Studies in 2006. She has 22 years of rehabilitation experience and has been a faculty member at LSU Health in Shreveport since 1997. She has presented research nationally and internationally on cultural competence, health disparities, wellness, and neurorehabilitation. She was honored by Maybelline as outstanding female educator and featured in People December 2006 issue. Dr. Morgan was also the 2014 recipient of the Allen A Copping Teaching Award, a finalist for the 2011 International Award for Research and recipient of the APTA Minority Faculty National Scholarship in 2003.
Abstract:
Introduction: Individuals with spinal cord injury (SCI) face health disparities and a number of challenges in maintaining cardiovascular health compared to the able bodied population. The causes are multifactorial including susceptibility to numerous medical conditions that impart a health hazard; illness behaviors leading to a disproportionate percentage of deaths as a result of preventable causes and changes in the ability to exercise to maintain heart health. Therefore, establishing and providing effective interventions for individuals with SCI is vital, however, the majority of rehabilitation research has been performed in research laboratories.
Aim: Aim of this study is to identify the possible physiological adaptations gained from utilizing a functional electrical stimulation (FES) bike for aerobic conditioning to address the increased prevalence of cardiovascular risk factors exhibited by the chronic SCI population, ASIA A-D in an outpatient clinic setting.
Methods: Single-subject case study involved an individual with tetraplegia, enrolled in an outpatient wellness program. Participant engaged in a cardiovascular endurance exercise program using an FES bike 30 minutes, three times a week for six months in a clinical setting, supervised by a physical therapist. The following variables were measured at baseline and at the end of the six months intervention: Hemoglobin A1c, cholesterol (total, HDL/LDL ratio), and serum triglycerides.
Results: Participant’s A1c, LDL cholesterol and triglycerides decreased and HDL cholesterol increased after six months of intervention.
Conclusion: Cardiovascular conditioning with an FES bike conducted in an outpatient setting can reduce cardiovascular risk factors and facilitate health in individuals with chronic SCI.
Sibel Catirli Enar
Turkiye Hospital, Turkey
Title: The right heart in heart failure with preserved ejection fraction
Time : 15:35-16:00

Biography:
Sibel Catirli Enar graduated from Ä°stanbul University, Ä°stanbul Medical School in 1981. She is specialized in anesthesiology and critical care in Ä°stanbul Medical School in 1985 and in cardiology at Ä°stanbul University Ä°nstitute of Cardiology in 1992. She became Associate Prof.of Cardiology in 2000, Fellow of European Society of Cardiology in 2010, Fellow of American Society of Echocardiography in 2012, Fellow of International Society of Cardiac Ultrasound in2012 and Fellow of American College of Cardiology in 2016.Working at Turkiye Hospital and Memorial Hospital in Istanbul/Turkey since 2000. She worked as a research fellow in Cleveland Clinic of Foundation-USA 1996-1998 and in University of Alabama at Birmingham-USA 2006-2008 as well. She is the member of Medical Societies: Turkish Society of Cardiology, European Society of Cardiology (member of cardiac imaging (EACVÄ°), heart failure association and valvular heart disease groups), American Society of Echocardiography (ASE), American College of Cardiology (ACC), American Heart Association (AHA), Ä°nternational Society of Cardiac Ultasound (Ä°SCU). She is the author of a chapter in” Metabolic syndrome in women” (2015) and contributor in “Interesting Cases in Echocardiography”-(N.Nanda-2017). She is referee for scientific abstracts,member of scientific comittes and referee in scientific journals.Has taken part in multicenter studies. She has publications in National and International Journals. She served as speaker and moderator in National and International Congresses. Her area of interest is echocardiography.
Abstract:
Heart failure with preserved ejection fraction (HFpEF) affects nearly half of the patients with clinical signs of heart failure.HFpEF is considered to be a disease of the left ventricle (LV). It is characterized by impaired diastolic function due to to abnormal relaxation and increased chamber stiffness.The role of right ventricle (RV) has not been well characterized in HFpEF. Recently several studies have described the role of RV in these patients by echocardiography, and few studies by CMR. In these studies,it has been found that addition of RV dysfunction is related with worse prognosis. The following explanation has been proposed: Impaired LV diastolic function causes passive rise in left atrial (LA) pressure and consecutively in PAWP and pulmonary artery (PA) pressure. Pulmonary artery compliance (PAC) decreases and adds to the increasing resistance against the right ventricle.RV fails to compensate pressure overload,dilates and finally RV failure occurs.Left atrial dilation is also present in these patients. Although HFpEF is considered as a disease of the left ventricle,RV dysfunction is also affected. Diabetes Mellitus and hypertension present with HFpEF predominantly, however RV dysfunction is also observed in these patients. Improvement of right heart imaging by echocardiography and CMR will be very helpful in the diagnosis and determining the prognosis.
John J Wang
Philips Healthcare, USA & B Milan Horacek Dalhousie University, Canada
Title: Improved acute myocardial ischemia detection by vessel-specific leads (VSLs) derived from the 12-lead ECG
Time : 16:15-16:40

Biography:
John Wang received the M.S. degree in physics from Northeastern University, Boston, and the MS degree in aeronautics and astronautics from MIT, Cambridge. He has more than 30 years’ industrial experience in the development of patient monitoring devices and is currently a principal scientist with Philips Healthcare responsible for the development of ECG monitoring algorithms and related applications used in all Philips’ patient monitoring devices. He has over 50 publications and 9 issued patents. John is an AAMI ECG Committee member responsible for developing industry standards for ECG devices. He is also an editorial board member of the Journal of Electrocardiology and a referee for several biomedical signal processing journals and conferences. John has served as a chair/co-chair for a number of conferences and was also an organization committee member for three Computing in Cardiology annual meetings. John has also served as a consultant/reviewer for NIH on SBIR grant application.
Abstract:
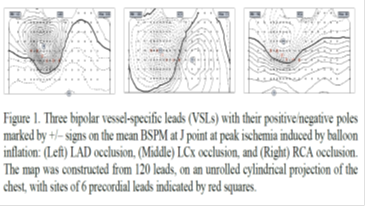
To further improve existing criteria recommended by ACC/ESC for identifying patients with ST elevation myocardial infarction (STEMI) from the 12-lead ECG, we have developed new criteria based on ST deviation calculated from 3 “optimal” vessel-specific leads (VSLs) derived from the 12-lead ECG. The performance of the VSLs vs. STEMI criteria was evaluated using two independent datasets of 12-lead ECGs: the Glasgow dataset included admission ECGs of 116 patients who were hospitalized for chest pain and underwent contrast-enhanced cardiac MRI that confirmed AMI in 58 patients (50%) and the Lund dataset included ECGs of 100 patients (75% males, age: mean/range 52/12-83 years) chosen to represent five subgroups with various causes of pathological ST-deviation, other than acute coronary occlusion: ventricular pre-excitation (n=12), acute pericarditis (n=26), ERS (n=14), LVH (n=26), and LBBB (n=22). Both STEMI criteria and VSLs method with and without an augmented LVH-specific derived lead were tested. Sensitivity (SE) and specificity (SP) were calculated and used as the performance measures for comparison. For the Glasgow dataset, STEMI criteria yielded SE/SP of 43/98%, whereas the VSLs improved SE/SP to 60/98%. The most significant increase in diagnostic performance appeared in patients with LCx occlusion (n=13): SE was improved from 31% to 69%. For the Lund dataset, SP test results using the STEMI and VSLs criteria were 100%/92%, 4%/88%, 29%/100%, 100%/96%, and 64%/68% for the five subgroups: pre-excitation, pericarditis, ERS, LVH, and LBBB, respectively. For the whole group, SP results were 57% for the STEMI criteria and 88% for the VSLs method. The performance improvement was statistically significant (p < 0.001). Based on these results we conclude that the new VSLs method has the potential to outperform the existing STEMI criteria in identifying patients who should receive emergent reperfusion therapy. This finding needs to be corroborated further on a larger study population.
References:
- Wang JJ, Pahlm, O, Wagner GS, Warren JW, Horacek BM, Sapp JL. Validation of the vessel-specific leads (VSLs) for detection of acute ischemia on a dataset with non-ischemic ST-segment deviation. J Electrocardiol 2016;49:800-806..
- Wang, J. Potential solutions for managing real-time ECG/arrhythmia monitoring alarms: A review. Computing in Cardiology 2016;43:301-304.
- Wang JJ, Title LM, Martin TN, Wagner GS, Warren JW, Horacek BM, Sapp JL. Validation of improved vessel-specific leads (VSLs) for detecting acute myocardial ischemia. J Electrocardiol 2015;48:1032-1039.
- Zong W, Kresge S, Lu H, Wang J. A real-time ST-segment monitoring algorithm based on a multi-channel waveform-length-transformation method for Q-onset and J-point detection. Computing in Cardiology 2014;41:641-644.
- Akil S, Al-Mashat M, Heden B, Hedeer F, Logi J, Wang JJ, Wagner GS, Warren JW, Pahlm O, HoráÄek BM. Discrimination of ST deviation caused by acute coronary occlusion from normal variants and other abnormal conditions, using computed electrocardiographic imaging based on 12-lead ECG. J Electrocardiol 2013;46:197-203
Alex Mota Benevides
Federal University of ABC, Brazil
Title: The greater the excess weight, the higher are the chances of having associated diseases that elevate the risk of acute myocardial infarction
Time : 16:40-17:05

Biography:
Alex Mota Benevides is a Cardiovascular Surgeon, completed his Graduation in Medicine at Federal University of Pará. He has a specialization in Cardiovascular Surgery at Beneficência Portuguesa de São Paulo. He is currently a Professor and holds a Master's Degree in Health Sciences at Faculty of Medicine of ABC, Brazil.
Abstract:
Introduction & Aim: Several studies demonstrate the relationship between obesity and the development of several diseases, including the National Health and Nutrition Examination Survey III. Pathologies as hypertension, type 2 diabetes mellitus and dyslipidemias are associated with a higher risk of cardiovascular diseases (CVD), among them acute myocardial infarction. This study aims to evaluate the relationship between the Body Mass Index (BMI) and the presence of diseases that increase the risk of CVD.
Methods: 187 patients were studied, individuals obtained by a spontaneous membership, among which, 48.6% were between 35 and 44 year old and 86.6% were female. This is a cross-sectional, descriptive and analytical statistical study, and the statistical tests (odds ratio) grants to reach 95% as the range of confidence.
Results: According to the classification of BMI, 44% of the participants had overweight, 22.6% obesity grade I, 22% normal BMI, 7.5% obesity grade II and 3.5% obesity III. The group with a BMI of 30 kg/m2 or higher, presented the highest prevalence of associated diseases: 52.4% of those had one or more comorbidity already installed. The odds of developing diseases in those presented 3.9 times (CI 1.61-9.52) higher when compared to normal BMI individuals (p=0.002). When we did this relation, according to the degree of obesity, we observed that the odds were 3.55 times (CI 1.37 -9.24) higher for those with obesity I (p=0.008). For those with obesity II were 3.56 (CI 0.99-12.82), (p=0.046), for those with obesity III, these odds increased to 8.9 (CI 1.47-53.71) with p=0.008.
Conclusion: The higher the BMI classification the higher prevalence of comorbidities that increase the chances of developing CVD, the fight against obesity seems to be a good strategy for the prevention of associated diseases and changes in lifestyle are fundamental to reduce the incidence of CVD in the population.
References:
- World Healthy Organization. WHO.
- Brasil. Ministério da Saúde. Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico. Vigitel 2014.
- USA. CDC/National Center for Health Statistics. National Health and Nutrition Examination Survey. URL: https://www.cdc.gov/nchs/nhanes/
- Masters RK, Powers DA. Link BG.Obesity and US Mortality Risk Over the Adult Life Course. American Jnl of Epidemiology. Volume 177, Issue 5. 2012. Pp. 431-442
- Corrada MM, Kawas CH, Mozaffar F, et al. Association of body mass index and weight change with all-cause mortality in the elderly. Am J Epidemiol2006;163(10):938-949.
Guy Hugues Fontaine
Universite Pierre et Marie Curie & La Salpetriere Hospital, France
Title: Atrial dysplasia and the high frequency of atrial fibrillation in ARVD patients
Time : 17:05-17:30

Biography:
Guy Hugues Fontaine has made 16 original contributions in the design and the use of the first cardiac pacemakers in the early 60s. He has serendipitously identified ARVD during his contributions to antiarrhythmic surgery in the early 70s. He has developed the technique of fulguration to replace surgery in the early 80s. He has been one of the “216 individuals who have made a significant contribution to the study of cardiovascular disease since the 14th century”, one of the “500 greatest geniuses of the 21th century” (USA Books), one of the “100 life time of achievement” (UK Book). He has 900+ publications including 201 book chapters. He is a Reviewer of 21 scientific journals both in basic and clinical science. He has developed new techniques of hypothermia for neurologic brain protection in OHCA, stroke and spinal cord injury. He has also recently invented a high-tech device which can be considered as the ultimate in palliative care.
Abstract:
Introduction: Tonet et al. from Paris were the first to demonstrate a susceptibility of arrhythmogenic right ventricular dysplasia (ARVD) patients to supraventricular tachyarrhythmias. This concept was confirmed on larger series of ARVD patients from the USA and Switzerland. It was also observed by the senior author that atrial fibrillation/tachyarrhythmias (AF/AT) could be the first presentation of the disease. It was therefore, logical to study the atrial pathology of three ARVD patients who died of a non-cardiac cause. This abstract is the first to present the atrial histology of ARVD patients with comparison to healthy controls considering the typical histologic changes known in the RV in ARVD.
Methods: Histology of the right atrium (RA) was available in only three cases from a series of 73 ARVD patients, in whom ARVD was confirmed by pathology. The observed anomalies were adipocytes in two cases, interstitial fibrosis in all, associated with replacement fibrosis in one case. This prompted us to study the RA structure in four subsequent control patients without cardiovascular disease. Light microscopic examination with Leica digital image processing was performed. Staining was performed with HPS in ARVD to improve identification of fibrosis, and HE in the control group.
Results: The atrial pathology of all of these so-called normal individuals presented anomalies, which can be interpreted as the background of an atrial arrhythmogenic substrate similar to the recently reported pathology of the RV in ARVD. As such, we found adipose tissue, interstitial and replacement fibrosis including one case of lymphocytic infiltration in the atria of these healthy controls, like histologic changes of the RV observed in ARVD. Furthermore, we identified a perpendicular orientation of atrial myocardial fibers.
Discussion: The interface between the two perpendicular layers can be a zone of weakness leading to fat and fibrosis, particularly if increased loading conditions are present. Desmosomal variants may enhance this remodeling. However, since desmosomal mutations have not been observed in the normal heart, it is therefore possible to consider other genes or post-translational modification to underlay these changes. The unexpected results of this preliminary study need further confirmation. However, we propose new mechanisms including the role of active as well as healed myocarditis which may precede the development of AF/AT and explain why these arrhythmias are the most frequent in the human species.
Conclusions: The same pathological substrate of ventricular myocardium in ARVD is also extending to the atrium explaining the high frequency of AF in ARVD patients.
- Cardiac Surgery | Heart Failure | Myocardial Infarction | Sports Cardiology | Cardio-Oncology | Case Reports on Cardiology
Location: Amphi Theatre

Chair
Aris Lacis
Children Clinical University Hospital, Latvia

Co-Chair
Marco Piciche
San Camillo-Forlanini Hospital, Italy
Session Introduction
William E Feeman Jr.
Wood County Hospital, USA
Title: Statin therapy in a 101 year old survivor of myocardial infarction
Time : 10:20-10:45

Biography:
William E Feeman is a Physician at Wood County Hospital. He is the Founder of Association for the Prevention of Atherothrombotic Disease in Northwest Ohio to facilitate the spread of knowledge about this disease.
Abstract:
There is not a consensus of opinion on statin therapy of dyslipidemia in the oldest of the very of patient population. This is a case report of a 75 year old woman who sustained an acute myocardial infarction. Because her attending physician did nothing in the way of treating her dyslipidemia, the patient began to attend the author’s clinic. She started to take stain therapy and aspirin. Her initial course was marked by recurrent chest pains, and a calcium channel blocker was added. The chest pains subsequently resolved and the patient has done well on super-stain therapy, combined with aspirin and calcium channel therapy—with no other interventions, medical or surgical. She is doing well, living in her own home, at age 101½ years. This is a report of a unique case showing that optimal medical therapy including super-stain therapy can be effective in controlling dyslipidemia even in the oldest of the very old patients with dyslipidemia.
Reda Biomy Mohamed
Benha University, Egypt
Title: Effect of chronic hepatitis C virus treatment by combination therapy on cardiovascular system
Time : 11:00-11:25

Biography:
Reda Biomy completed his Graduation at Benha University, Egypt and MD in Cardiology 1992. In 1995, he worked as an Associate Professor of Cardiology at Benha University, Egypt and he was responsible for non-invasive cardiology lab and cardiac catheterization lab.
Abstract:
Introduction: The prevalence of hepatitis C virus (HCV) in Egypt is quite high and the recent introduction of combined oral direct antiviral agents may have impressive results.
Aim: Aim of this study is to assess the cardiovascular effects of direct acting antiviral agents (DAAs) in combination with or without pegylated interferon alpha (PEG-IFN) in Egyptian patients with chronic hepatitis C infection.
Methods: This study included 170 patients suffering from chronic hepatitis C virus infection. Patients were divided into two groups; first group (100 patients) received triple combination therapy in the form of pegylated interferon alpha, sofosbuvir (sovaldi) and ribavirin, while second group (70 patients) received dual combination therapy in the form of sofosbuvir and simeprevir (sovaldi and olysio). Group one patients were followed up for one year over three visits; before initiating treatment, then six months and 12 months later while group two patients were followed up for six months over two visits; before initiating treatment and then six months later and the end point of the study was either development of a major cardiovascular event throughout the course of the study (e.g. congestive heart failure, echocardiographic evidence of LV dysfunction, occurrence of significant arrhythmias or acute coronary syndrome) or completing till the end of the study without any evidence of cardiac affection. The following parameters were accomplished, thorough medical history and clinical examination, ECG, echo-Doppler study and laboratory investigations.
Results: No significant differences were found between the two study groups as regards demographic criteria. None of both group patients had developed any major cardiac event (e.g. congestive heart failure, echocardiographic evidence of LV dysfunction, occurrence of significant arrhythmias or acute coronary syndrome). No significant changes as regards ST-T wave abnormalities or arrhythmias had occurred six and twelve months after initiation of treatment compared to baseline visit. None had developed prolonged QT interval at follow up visit. No significant changes were seen in the mean values of corrected QT in group two patients over study visits (p value>0.05). None of both group patients had or developed echocardiographic regional wall motion abnormalities (RWMA) at baseline or at study end. Systolic function parameters showed minute non-significant changes over study visits (p value>0.05). Diastolic function parameters (E/A ratio, deceleration time and E/Ea ratio) showed non-significant changes between baseline and 6- and 12 month visits (p value>0.05).
Conclusion: The direct antiviral agents used in combination regimen with interferon (pegylated interferon alpha, sofosbuvir and ribavirin) or used orally in combination (sofosbuvir and simeprevir) not significantly affect the cardiovascular system.
Aris Lacis
Children Clinical University Hospital, Latvia
Title: Using stem cells for stimulating tissue regeneration and functional activity in a wide spectrum of pathologies
Time : 11:25-11:50

Biography:
Aris Lacis is a Cardiac Surgeon and Professor. He completed his Graduation at Riga Medical Institute in 1961. He was a General and Thoracic Surgeon at P. Stradins University Hospital in Riga (1964–1969); Thoracic and Cardiac Surgeon at Latvian Centre for Cardiovascular Surgery (1969–1994) and; Head of Pediatric Cardiology and Cardiac Surgery Clinic at University Children’s Hospital, Riga (1994-2012). He is the President of Latvian Association for Pediatric Cardiologists, Author of 395 scientific publications, three monographs and 13 patents. He is an Investigator of more than 10 clinical trials including Cardio-surgical procedures performed under deep hypothermia and hybrid procedures etc.
Abstract:
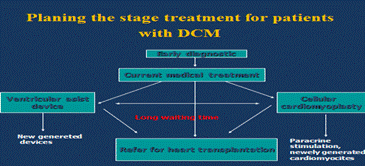
Statement of the Problem: Dilated cardiomyopathy is a serious problem in pediatric cardiology praxis. Despite the relatively low incidence of 0.57 to 2.6 per 100000 children, the mortality rate is high. One third of patients die within the first year after diagnosis. Up to 40% of these patients are defined as idiopathic dilated cardiomyopathy (IDCM), characterized by ventricular dilation and systolic dysfunction. Researchers have reposted that conventional medical therapy does not improve the outcome of the disease; however, recent clinical studies have suggested bone marrow derived autologous mononuclear cells as a promising therapy option. Pulmonary arterial hypertension (PAH) is characterized by increased pulmonary vascular resistance resulting in extensive heart structural changes leading to right heart failure and death. PAH is characterized by obstruction of small pulmonary arteries leading progressive increase in vascular resistance. Locally implanted stem cells may trigger the neovascularization process in the lung potentially leading to a decrease of pulmonary artery pressure.
Methodology: For treatment of IDCM, we prefer to use transcutaneous intramyocardial administration of autologous bone marrow derived mononuclear stem cells, combined with ultrasound monitoring. In patients with PAH intrapulmonary transplantation of stem cells was performed using intravasal injection of the stem cells by catheterization pulmonary arteries and directly in the lung tissues by using standard thoracentesis technique, performed under chest radiological control.
Conclusions: If applied wisely, the stem cell therapy appears to be a safe and effective way for stabilization of critically ill patients with both severe pulmonary arterial hypertension and idiopathic dilated cardiomyopathy. This method provides additional opportunities for symptomatic treatment and serves as a bridge for potential heart and lung transplantation.
References:
1. “Intramyocardial administration of autologous bone marrow mononuclear cells in a critically ill child with dilated cardiomyopathy”. LÄcis A., Ä’rglis A. Cardiology in the Young, 2011, 21, 110–112
2. “Neo-revascularization as the potential treatment for patientsuffering from pulmonary hypertension (Myth or reality?)” LÄcis A., Lubaua I., Ä’rglis A. et al. J. Clinical Medicine Research (CMR), 2013, 2 (3): 32–36
3. “Management of idiopathic dilated cardiomyopathy with intramyocardial cell transplantation in children. A retrospective study of 7 patients” LÄcis A., Lubaua I., Ä’rglis A. et al. J. Clinical Medicine Research (CMR), 2013, 2 (4): 129–133
4. “Safeguards and pitfalls in technique used for stem cell delivery in children suffering from idiopathic dilated cardiomyopathy” LÄcis A., Lubaua I., Ä’rglis A. et al. Journal of US-China Med. Science, 2013, vol. 10, N 3–4, 71–75
5. “Stem cell therapy as one of temporary measures for management of heart failure and pulmonary hypertension in children” LÄcis A., Lubaua I., Ä’rglis A. et al. American Journal of Experimental and Clinical Research, 2014, 1 (3): 38–46
Marco Piciche
San Camillo-Forlanini Hospital, Italy
Title: The nature and enigma of the noncoronary collateral circulation
Time : 11:50-12:15

Biography:
Marco Piciche completed his Graduation in Medicine at University of Florence in 1995 and Cardiac Surgery Residency at Tor Vergata University of Rome in 2000. He has worked as an Assistant at Saint Luc Hospital, Catholic University of Louvain, Brussels (1999–2001), as a Clinic Head/Hospital Assistant at universities of Clermont-Ferrand (2003–2004) and Montpellier (2004–2007). In Canada, he authored a research project on ‘‘Noncoronary collateral circulation,’’ which was submitted to the annual research competition at Québec Heart & Lung Institute, Laval University, and received the competition’s highest grant. In September 2011, he completed his PhD in Therapeutic Innovations from Paris-Sud University. He is the Editor in Chief of the book Dawn and Evolution of Cardiac Procedures-Research Avenues in Cardiac Surgery and Interventional Cardiology. Currently, he is a Consultant Cardiac Surgeon in Italy.
Abstract:
Notwithstanding the fact that the coronary collateral circulation (CCC) is the only blood supply warranting ongoing attention, the human heart benefits from a small additional source of blood, called noncoronary collateral myocardial blood flow (NCCMBF) or noncoronary collateral circulation (NCCC). It consists of a small blood supply reaching the heart through a micro-vascular network arising from the bronchial, esophageal, pericardial and diaphragmatic arteries. These small channels enter the heart through the pericardial reflections surrounding the pulmonary and systemic veins, connecting with the vasa vasorum of the aorta and pulmonary artery. The left and right internal mammary arteries (ITAs), along with their collateral branches, are among these non-coronary sources. Under certain circumstances the ITAs have a high potential for developing collateral branches. In the case of severe Leriche syndrome or with chronic obstruction of the abdominal aorta, the ITAs can serve as the main or even sole source of blood supply to the lower limbs. Communication is also possible between the ITAs and the native coronary arteries. This has been demonstrated by angiography in living patients, both for right and left coronary artery disease. Postmortem angiography in patients with ischemic heart disease has demonstrated such connections in 12% of cadavers. The Vineberg operation of the 1940s was based on the plastic potential of the ITAs. It consisted of ITA implantation into the left ventricular wall, with development of an extensive collateral network visible at angiography even at very long-term follow-up. It has been recently demonstrated that in ischemic conditions there is a functional, ischemia-reducing extracardiac coronary artery supply via natural ipsilateral ITA anastomosis. Herein, the available data on the non-coronary blood supply to the human heart have been reviewed.
References:
- Picichè M. Noncoronary Collateral Myocardial Blood Flow: The Human Heart’sForgotten Blood Supply. The Open Cardiovascular Medicine Journal, 2015, 9, 105-113
- Picichè M, Kingma JG, Voisine P, Dagenais F, Fadel E. Angiogenesis and surgical or endovascular enhancement of noncoronary collateral circulation: A new research field. J Thorac Cardiovasc Surg 2010; 139 (6): 1675-6.
- Picichè M, Kingma JJ, Fadel E, Dagenais F, Mathieu P , Simard D, De Maria RG, Voisine P. Enhancement of noncoronary collateral blood flow from the internal thoracic arteries: the theoretical and practical basis of an alternative method of myocardial blood supply. J Cardiovasc Surg 2011; 52(1):127-31
Rachad M Shoucri
Royal Military College of Canada, Canada
Title: A look at heart failure based on the study of end-systolic pressure-volume relation (ESPVR)
Time : 12:15-12:40

Biography:
Rachad M Shoucri completed his BSc in Electrical Engineering at Alexandria University, Egypt; MSc in Optical Physics and; PhD in Theoretical Physics at Laval University, Québec, Canada. After graduation in 1975, he worked for five years at the Hôpital Saint-Sacrement and the Institut de Cardiologie de Québec where he developed his current interest in Mathematical Physiology and in the application of mathematics in cardiology. Since 1981, he is working in Department of Mathematics and Computer Science at Royal Military College of Canada, Kingston, Ontario.
Abstract:
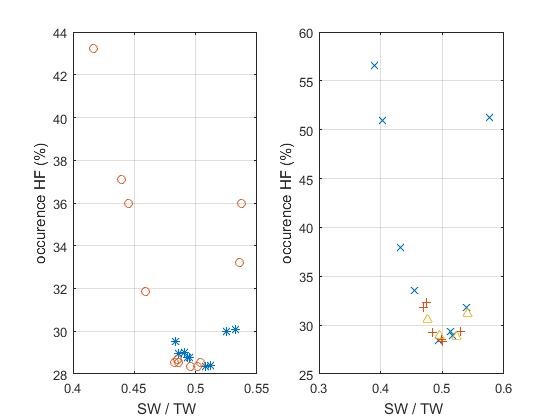
Parameters describing the linear and non-linear models of the end-systolic pressure-volume relation (ESPVR) in the heart ventricles have been derived, relations of these parameters with the ejection fraction (EF) have been obtained. The relations between the parameters of the ESPVR and EF can be applied to the study of the problem of heart failure with reduced or preserved EF (HFpEF). The results of this study show that important information concerning the problem of HFpEF can be derived from the parameters describing the ESPVR. Applications to clinical data published in the literature show the consistency of the mathematical formalism used to calculate the equation of the non-linear ESPVR in which formalism is based on the theory of large elastic deformation of the myocardium. The results presented in the figures show one possible application, the relation between the percentage occurrence of heart failure (HF) and the ratio SW/TW (SW=stroke work, TW=total area under the ESPVR). The results are presented on two figures for the purpose of clarity for five clinical groups: normal*, aortic stenosis o, aortic valvular regurgitation +, mitral regurgitation ^, miscellaneous cardiomyopathies x. Note that both curves have a minimum around SW/TW≈0.5. Note also that the normal group (*) appears near the minimum of the curve on the left hand side (corresponding to EF≈0.67). The case of aortic stenosis on the left hand side appears in three subgroups. Calculation indicates an optimal value of SW/SWx≈0.8 (SW=stroke work, SWx=maximum stroke work corresponding to a given ESPVR). The quantity SWR=SWx–SW is the stroke work reserve; we have calculated SWR/SW≈0.25 for SW/TW≈0.5.
References:
- Dumesnil JG, Shoucri RM, Laurenceau JL, Turcot J (1979) A mathematical model of the dynamic geometry of the intact left ventricle and its application to clinical data. Circulation 59: 1024-1034
- Shoucri RM (2010) ESPVR, ejection fraction and heart failure. Cardiovasc. Eng. 10: 207-210.
- Shoucri RM (2015) End-Systolic Pressure-Volume Relation, Ejection Fraction, and Heart Failure: Theoretical Aspect and Clinical Applications. Clinical Medicine Insights: Cardiology 9(S1): 111-120.
- Da Mota JPGF (2013) Intelligent modeling to predict ejection fraction from echocardiographic reports. MSc thesis in Mech Eng, IST Técnico Lisboa, Portugal.
- Curtis JP, Sokol SI, Wang Y, Rathore SS, Ko DT, et al (2003) The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J Am Coll Cardiol 42 (3): 736-742.
Fabiola B Sozzi
University Hospital Policlinico of Milan, Italy
Title: Congenital coronary fistulae: Clinical impact and interesting cases
Time : 12:40-13:05

Biography:
Fabiola B Sozzi works as a Staff Cardiologist at University Hospital Policlinico of Milan, Italy. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She has expertise in Echocardiography at Thoraxcenter of Rotterdam (NL), where she defended her PhD thesis on Stress Cardiac Imaging under the supervision of Professor J Roelandt. She is a Visiting Professor at University of Milan where she leads several research projects and teaches at Faculty of Medicine and School of Specialization of Cardiology. She is an Author of 70 papers published in peer-reviewed international journals and Reviewer of several medical international journals.
Abstract:
Coronary fistulae (CAF) with the cardiac chambers are extremely rare congenital vascular anomalies, reported in approximately 0.08-0.3% of unselected patients. Although coronary artery fistulae are commonly asymptomatic, they may cause severe symptoms depending on the severity of the shunt. Little data on the clinical impact and treatment are available. We aim to determine the outcome of percutaneous closure of large hemodynamically significant CAF in young patients. We retrospectively analysed 11 patients (median age at intervention 21 years, three females) affected by relevant congenital CAF, diagnosed by echocardiogram and cardiac catheterization. All patients underwent percutaneous closure and were followed for a mean period of three years. The clinical presentation of CAF was characterized by symptoms. In some cases CAF was incidentally diagnosed by echocardiogram. Most fistulas were originating from the left coronary artery (LCA) [7/11]. The right heart was the most common site of drainage (8/11). Multiple fistulas were found in three patients. No-one had other congenital disorders associated. All patients were treated with percutaneous transcatheter embolization. During follow-up, no patient died. In one case a retrograde thrombosis of the fistula with acute myocardial infarction occurred after one month and was treated with thrombectomy and coronary bypass. No other major adverse cardiac events were recorded. We conclude that the percutaneous closure of significant CAF is associated with low event-rate and excellent prognosis. A rich iconography based on echocardiography, computed tomography, magnetic resonance imaging and angiography are presented for some interesting cases.
- Workshop on: "Torsades de Pointes (TdP)"
Location: Amphi Theatre
Session Introduction
Guy Hugues Fontaine
Universite Pierre et Marie Curie & La Salpetriere Hospital, France
Title: Torsades de Pointes (TdP)
Time : 14:05-15:05

Biography:
Guy Hugues Fontaine has made 16 original contributions in the design and the use of the first cardiac pacemakers in the early 60s. He has serendipitously identified ARVD during his contributions to antiarrhythmic surgery in the early 70s. He has developed the technique of fulguration to replace surgery in the early 80s. He has been one of the “216 individuals who have made a significant contribution to the study of cardiovascular disease since the 14th century”, one of the “500 greatest geniuses of the 21th century” (USA Books), one of the “100 life time of achievement” (UK Book). He has 900+ publications including 201 book chapters. He is a Reviewer of 21 scientific journals both in basic and clinical science. He has developed new techniques of hypothermia for neurologic brain protection in OHCA, stroke and spinal cord injury. He has also recently invented a high-tech device which can be considered as the ultimate in palliative care.
Abstract:
Torsades de Pointes (TdP) is a rare but important cause of sudden death of young people with the genetically determined long or short QT syndrome. The length of the QT interval is directly related to the risk stratification of these patients modulated by genetic factors. TdP is also a major concern of the pharmaceutical industry for the development of any cardiac and even non-cardiac drugs. Endocardial recordings during TdP in human have brought new concepts for the understanding of this arrhythmia mechanism. Here, presence of intramyocardial conduction defects is demonstrated by the analysis of endocardial potentials observed on the QRS complexes in complete AV block. We present for the first time that patients (old females) with spontaneous complete AV block have a trouble in conduction not only on the AV conduction system but also inside the myocardium. This concept is reinforced by the absence of EGM but only far field potentials observed several times presented in a unique case. These images document the concept of depressed myocardium in which not only AV conduction but also intramyocardial conduction is impaired. It may explain that most TdP are transient and return spontaneously to sinus rhythm. Other data have demonstrated the presence of Wenckebach type I and Mobitz type2 in the myocardium of those patients suggesting that the myocardium has preferential pathways working as conduits transmitting ventricular activation. This is also in agreement with the identification of a specific genetic background.
- Heart Failure | Myocardial Infarction | Cardiac Surgery | Sports Cardiology | Cardio-Oncology | Case Reports on Cardiology
Location: Amphi Theatre

Chair
Aris Lacis
Children Clinical University Hospital, Latvia

Co-Chair
Marco Piciche
San Camillo-Forlanini Hospital, Italy
Session Introduction
Jean-Pierre Usdin
American Hospital of Paris, France
Title: Cardio-oncology, a medical speciality for these linked pathologies
Time : 15:05-15:30

Biography:
Jean-Pierre Usdin is a former Internal of the Hospitals of Paris, former Head of clinic, Assistant of hospitals of Paris, former Consultant of scientific committee of medical journal Consensus and previous Chief of the Cardiologic department of American Hospital of Paris (2006-2012). He is currently renowned Cardiologist at American Hospital of Paris, member of European Society of Cardiology and member of French Society of Cardiology. Being a Journalist and Blogger in Medscape France from 2010, he has blogs dedicated to general cardiology: Reports discussions and notes about trials, cardiology congresses, live-comments on 2015 ESC Congress in London.
Abstract:
Cardiovascular diseases and cancer are the leading causes of death from non-communicable diseases in the world. These two top killers share not only this characteristic but have common specificities. Risk factors are some modifiable: Tobacco, social custom sedentarity, environment, others are not: Age, heredity. Cardiovascular health cancer therapies occupy an important place. As cancer therapies are more and more active, affected people are cured or living longer, so heart disease is an emerging problem in this population. For this purpose a sub speciality: Cardio-oncology was created. Cardio oncology permits specialists of cardiology and oncology not only to share the immediate but the long term of illnesses. As example, in the past, we all know the effects of chemotherapy (anthracyclines) on myocardial function, the occurrence of constrictive pericarditis many years after chest radiotherapy. But new cancer treatments like immunotherapy, hormonotherapy, cell specific inhibitor antibodies, are no safer and interfere with heart and vascular function. According to my knowledge, there is no cardiologist regularly invited in multidisciplinary staff meetings, debating pros and cons of patient’s treatments. On the other side, cardiac therapies are sometimes pointed out to provoke (statin) or protect from (aspirin) cancer when prescribed on a long term basis. Cardio oncology speciality will permit in the very next future to unify in one specialist the treatment of these frequently associated pathologies.
Syed M S Mujtaba
Freeman Hospital, UK
Title: Extended trans-septal versus left atrial approach in mitral valve surgery: 1017 patients experience
Time : 15:30-15:55

Biography:
Syed M S Mujtaba completed his Graduation at Dow Medical College, Karachi, Pakistan in 1985. He did his basic and higher Surgical training in Ireland and FRCS in 1993. He started Cardiothoracic Surgery at University Hospital Cork, Ireland in 1994. In 1997, he started his training in Cardiothoracic Surgery at Yorkshire Heart Centre, Leeds, UK. He worked for two years in Dubai as Senior Registrar. He joined as Consultant Cardiac Surgeon at Liaquat National Hospital, Karachi, Pakistan and worked for three years. Then, he worked as Consultant in Tabuk, Saudi Arabia for 18 months and as Medical Director at Baqai Centre for Cardiovascular diseases, Karachi for a year.
Abstract:
Statement of the Problem: The mitral valve may be accessed directly through the left atrium but visualization can sometimes be challenging. A trans-septal inter-atrial approach provides better exposure and easy access for concomitant tricuspid procedures especially in difficult cases. This retrospective study evaluates the safety and effectiveness of the extended vertical trans-septal approach for routine mitral valve exposure.
Methodology & Theoretical Orientation: 1017 consecutive patients undergoing an isolated primary mitral valve procedure (repair/replacement) through a median sternotomy were retrospectively studied between 2000 and 2015. 135 patients were operated by extended vertical trans-septal approach (EVTSA, group A) while 882 patients underwent a traditional left atrial (LA, group B) approach.
Findings: There were 135 patients (M/F=56/79) in group A and 882 patients (M/F=398/484) in group B. Logistic EuroSCORE was significantly lower in EVTSA group (0.61 vs. 0.90 p=0.000001). In the LA group, there were more patients with pre-operative TIA or stroke (94 vs. 6, p=0.005). Cumulative cross clamp time was 82 (44-212) minutes (EVTSA) and 78 (30-360) minutes (LA) groups (p=0.271) while cardiopulmonary bypass time was 107 (58-290) and 114 (43-602) minutes respectively (p=0.121). Post-operative blood loss was 415 ml (EVTSA) versus 427(LA) ml (p=0.273). No significant difference was found in the incidence of post-operative atrial fibrillation (p=0.22) or heart block requiring permanent pacemaker (p=0.14).
Conclusion & Significance: An extended vertical trans-septal approach to the mitral valve is safe and reproducible. It gives excellent exposure of the mitral valve under all circumstances without any significant increase in cross clamp or bypass time, post-operative arrhythmia, heart block/pacemaker rate or bleeding.
Porawan Bunleng
Bumrungrad International Hospital, Thailand
Title: Strategies for improving door-to-ECG time in acute coronary syndrome patients: Bumrungrad International Hospital
Time : 16:10-16:35

Biography:
Porawan Bunleng completed her Graduation at Faculty of Nursing, Khon Kaen University. She has 15 years of experience in Nursing and eight years of experience at Heart Center, Bumrungrad International Hospital. She has an experience of Supervising and Overseeing the Nursing department to meet the specified goals; controlling service standards; administering the organizational and personnel works and managing the medical supplies to meet the policy; reviewing administrative process and procedures to achieve efficient results.
Abstract:
Background: Target ACS is a hospital quality initiative by setting challenging target for achieving the door-to-ECG time goal of 8 min ACS patients (The goal standard of door-to-ECG time benchmark is <10 min). Our hospital’s STEMI sub-committee recognized the importance of improving door-to-ECG times due to the benefit of a rapid initial ECG results can lead to rapid reperfusion.
Aim: Aim of this study is to improve door-to-ECG time for achieving door-to-ECG time goal of 8 min in ACS patients.
Methods: This study was conducted at the Bumrungrad International Hospital, Thailand. This hospital has 580 in-hospital beds and emergency cardiac catheterization is available 24 hours. Multi-component strategies includes: Provide infrastructure in an especially high-risk area for heart attack in hospital to facilitate early identification of critical arrhythmias such as ECG monitoring, fast track communication, etc.; develop a standardized annual education program to ensure ongoing competency in ECG acquisition skill to identify STEMI patients in the field; having a dedicated quality assurance process to monitor performance of the STEMI bypass system, and; a real time dashboard to monitor STEMI performance and using for gap analysis based on a comparison of current practice and best practice to development of consensus recommendations for improvements in the management of STEMI patients in hospital.
Results: A total of 257 patients included in the study: 112 before (January to December 2014) and 145 after intervention (January to December 2016). Before the intervention, 48% received an ECG at 8 min or less. After the intervention, 97% met the time requirement, for a mean difference of 49%. The mean (min-max) time from door-to-ECG was decreased by 4 min after the intervention.
Conclusions: The overall percentage of patients with a door-to-ECG time within 8 min improved without increasing staffing.
Maja Karaman Ilic
General Hospital Sveti Duh & Josip Juraj Strossmayer University of Osijek, Croatia
Title: Non-invasive postoperative extravascular lung water monitoring
Time : 16:35-17:00

Biography:
Maja Karaman Ilic is an Anesthesiologist subspecialized in Intensive Care. She is dealing with perioperative fluid management for an extensive period of time. She has completed PhD in the field of Anesthesiology. She is experienced in using ultrasound in a diagnostic and therapeutic way for critical care patients.
Abstract:
Statement of the Problem: Pulmonary complications that occur after major thoracic and abdominal surgical procedures are the primary reason for extending a patient's stay in the intensive care unit. Complications range from atelectasis and pulmonary edema to pneumonia, acute lung injury and acute respiratory distress syndrome. Fluid replacement therapy is unavoidable during surgery. Too much fluid can cause rise in extravascular lung water (EVLW) and result with pulmonary edema. Assessment and monitoring of EVLW traditionally has relied upon invasive computed tomography (CT) or pulse counter cardiac output (PiCCO) testing. A less invasive and accurate alternative is the PaO2 to FiO2 (P/F ratio). A potentially sensitive non-invasive procedure for EVLW rise detection during early postoperative period is lung ultrasound.
Methodology & Theoretical Orientation: Since ultrasound waves are completely reflected by air, they can image the parenchyma only when interstitial-alveolar imbibition occurs. This gives rise to characteristic vertical artifacts called “B-lines”. The number of B-lines is directly proportional to the degree of lung aeration loss and to EVLW volume.
Findings: In our study, by use of lung ultrasound, volume small enough to produce shunting of ≤20% was detected before other clinical signs of EVLW rise.
Conclusion: Using lung ultrasound B-lines to detect EVLW has not been tested extensively, and it has not been compared with the conventional index of P/F ratio. If it allows accurate EVLW assessment, lung ultrasonography could become very useful tool in early detection and prevention postoperative pulmonary edema due to intraoperative fluid overload.
Syed M S Mujtaba
Freeman Hospital, UK
Title: Early clinical results of perceval suture-less aortic valve in 139 patients: Freeman experience
Time : 17:00-17:25

Biography:
Syed Saleem Mujtaba completed his graduation at Dow Medical College, Karachi, Pakistan in 1985 and; basic and higher Surgical training in Ireland and FRCS in 1993. He started Cardiothoracic Surgery at University Hospital Cork, Ireland in 1994. In 1997, he started his training in Cardiothoracic Surgery at Yorkshire Heart Centre, Leeds, UK. He worked for two years in Dubai as Senior Registrar. He was a Consultant Cardiac Surgeon at Liaquat National Hospital, Karachi, Pakistan and worked for three years. Then, he worked as Medical Director at Baqai Centre for Cardiovascular diseases, Karachi for a year. He worked as Clinical Fellow in Cardiothoracic Surgery for 18 months at Edinburgh Royal Infirmary in 2011. He moved to Freeman Hospital, Newcastle UK in March 2013 as Clinical Fellow and still working there. He completed his FRCS (CTh) in 2016.
Abstract:
Statement of the Problem: The aim of this retrospective study is to evaluate the safety and performance of the perceval suture-less valve in patients undergoing aortic valve replacement (AVR). We report the 30-day clinical, echocardiographic and hemodynamic outcomes of 139 patients.
Methodology & Theoretical Orientation: From January 2014 to December 2026, 139 patients underwent suture-less aortic valve replacement. Their operation notes, PACS records and per operative TOE findings were studied retrospectively. Patients with bicuspid aortic valve and abnormal STJ: annulus ratio was excluded.
Findings: 92 patients underwent isolated aortic valve replacement (group A) with perceval valve and 47 patients had combined procedures of AVR and coronary artery bypass grafting (group B). The patients received a size S (n=23), M (n=39), L (n=42) or XL (n=35) prosthesis. Perceval valve was successfully implanted in 135 patients (97.1%). Mean cross clamp and bypass time was 40 and 63 minutes for isolated cases, while it was 68 and 107 minutes for combined cases. Three patients (2.1%) died within 30 days. Four patients suffered stroke and five patients went into acute renal failure. Median ICU and hospital stay was 2 and 8.5 respectively. Four valves were explanted due to significant para-valvular leak after surgery. Five patients had permanent pacemaker as a result of complete heart block and mean post-operative drainage was 295 ml for isolated case and 457 ml for combined cases.
Conclusion & Significance: Early post-operative results showed that perceval valve is safe. It can be implanted with short cross clamp and bypass time. Further follow up is needed to evaluate the long-term outcome with this bio-prosthesis.
- Cardiovascular Risk| Rheumatic Heart Disease | Coronary Artery Bypass | Case Reports on Cardiology | Hypertension
Location: Amphi Theatre

Chair
Guy Hugues Fontaine
Universite Pierre et Marie Curie & La Salpetriere Hospital, France

Co-Chair
Reda Biomy Mohamed
Benha University, Egypt
Session Introduction
Anna Fratta Pasini
University of Verona, Italy
Title: Endoplasmic reticulum stress, Nrf2 signaling and cardiovascular diseases in a nutshell
Time : 10:55-11:20

Biography:
Anna Fratta Pasini is the Assistant Professor of Internal Medicine at University of Verona Medical School, Verona, Italy. She completed her MD degree at University of Verona. She is Board Certified Specialist in Gastroenterology at University of Verona and Board Certified Specialist in Endocrine Diseases at University of Verona. She is currently a board member of Verona University. She is the Editorial Board Member of Journal of Cardiology and Therapeutics and Journal of Geriatric Cardiology.
Abstract:
Endoplasmic reticulum (ER) stress is an adaptive mechanism that arises when excessive newly synthesized and/or misfolded polypeptides in the ER lumen exceed its protein folding capacity in response to multiple cellular stress triggers such as oxidative stress, hypoxia and hyperglycemia. The accumulation of unfolded/misfolded proteins activates transcriptional and translational pathways, known as the unfolded protein response (UPR), an adaptive response that helps cell survival by activating a series of intracellular signaling pathways. When the UPR fails to control the level of unfolded/misfolded proteins, ER-initiated apoptotic signaling is induced. Several studies have demonstrated that ER stress occurred in atherosclerotic plaques, particularly in the advanced stages. In addition, ER stress has an important role in cardiac hypertrophy mainly in the transition to heart failure. Interestingly, chronic UPR activation has also been observed in obesity and in diabetes. Oxidative stress that plays a key role in cardiovascular and metabolic disease is counterbalanced by complex antioxidant defense systems regulated by a series of multiple pathways, including the UPR, to ensure that the response to oxidants is adequate. Nuclear factor-E2-related factor (Nrf2) is an emerging regulator of cellular resistance to oxidants; Nrf2 is strictly interrelated with the UPR sensor called pancreatic endoplasmic reticulum kinase. Interventions against ER stress and Nrf2 activators seem to reduce myocardial infarct size and cardiac hypertrophy in animals and to protect against obesity and insulin resistance. These evidences may open new promising therapeutic approaches in chronic cardiovascular and metabolic diseases.
References:
- Ron D. Nat Rev Mol Cell Biol 2007; 8:519
- Back SH, Annu Rev Biochem 2012; 81:767
- Wang S, J Cell Biol 2012; 197:857
- Tabas I. Circ Res 2010; 107: 839
- Garbin U, Fratta Pasini A, Antiox & Redox Signal 2014; 21:850
- Cominacini L, Fratta Pasini A. Free Radic Biol Med 2015; S0891
- Pagliassotti MJ, Metabolism 2016; 65:1238
- Mozzini C, Fratta Pasini A, Free Radic Biol Med 2014; 68:178
- Singh S,Free Radic Res 2010;44:1267
- Digaleh H, Cell Mol Life Sci 2013; 70:4681
- Seo HA, Oxid Med Cell Longev. 2013; 2013:184598
Reda Biomy Mohamed
Benha University, Egypt
Title: Short-term outcome of balloon angioplasty of discrete coarctation of aorta
Time : 11:20-11:45

Biography:
Reda Biomy completed his Graduation at Benha University, Egypt and MD in Cardiology 1992. In 1995, he worked as an Associate Professor of Cardiology at Benha University, Egypt and he was responsible for non-invasive cardiology lab and cardiac catheterization lab.
Abstract:
Introduction: Balloon angioplasty has been proposed as an alternative way to surgery in primary treatment of aortic coarctation (CoA) for both children and infants.
Objective: The purpose of this study is to assess the immediate and intermediate term effectiveness and safety of balloon angioplasty in infants and children with native discrete membranous CoA.
Patients & Methods: 40 consecutive patients with native discrete coarctation of the aorta were treated with balloon angioplasty. They were eight infants and 32 children; with ages ranged from two months to 10 years and all weighted below 35 Kg. All patients were clinically evaluated immediately after and at six to 12 months and 18 to 24 months after the procedure. Follow up data were collected and Doppler echocardiography was done before intervention to confirm diagnosis and to plan management and post interventional to follow-up patients and estimate the outcome and complications.
Results: Immediate successful relief of native CoA was obtained in 92.5% of the population study, while 7.5% recorded immediate suboptimal results with pressure gradient above 20 mm HG. The peak systolic gradient across the coarcted segment was reduced significantly with 82.5% immediately after balloon angioplasty, 75% and 73.2% at the end of first and second follow up period respectively. Pressure gradient decreased significantly from 57±15.7 mm Hg before balloon angioplasty to 14.23±11.30 mm Hg 9 to 12 months after, but it was increased slightly to reach 15.15±11.80 mm Hg at the end of the second year. The systolic ascending aortic pressure decreased significantly (19%) and the systolic descending aortic pressure increased significantly (11.4%) at the end of the study. Recoarctation occurred in 17.5% at the end of the 1st year and balloon angioplasty was repeated for all patients successfully. At the end of the 2nd year, restenosis was evidenced in 10% of the whole study population at the site of coarcted segment occurred in 5%.
Conclusion: Balloon angioplasty is an effective and safe alternative to surgery for treatment of CoA in infants older than two months and children10 years of age or younger.
Philippe Chevalier
Louis Pradel Cardiology Hospital of Lyon, France
Title: Atrial structural remodeling gene variants in patients with atrial fibrillation
Time : 11:45-12:10

Biography:
Pr. Philippe Chevalier, MD PhD is the head of the Rhythmology unit of HCL and the coordinator of the National Reference Center for inherited arrhythmia. He is an internationally recognized clinical expert in the field of cardiac arrhythmias. He has been implicated in more than 10 clinical studies. He is the principal investigator and coordinator of a European multicenter study on molecular markers of sudden death. He develops fundamental studies on the pathophysiology of AF. He organized every year the national congress of “les journées de rythmologie” in Lyon. Regularly invited to international cardiology congress, he is also a member of several societies (French Society of Cardiology, American Heart Association). His research led him to be present in more than 200 publications in refereed journals.
Abstract:
Statement of the Problem: Atrial fibrillation (AF) is a common arrhythmia with a well-recognized inherited component. Until now, AF genetic studies mainly focused on the genes involved in electrical remodeling, rather than left atrial muscle remodeling.
Methodology: A high-throughput next-generation sequencing (NGS) workflow was developed based on a custom AmpliSeq™ panel of 55 genes potentially involved in atrial myopathy. This workflow was applied to a cohort of 94 patients with AF, 66 with atrial dilatation and 28 without. Patients with variants in the selected genes underwent further screening for pathogenic mutations in prevalent arrhythmia-causing genes. Bioinformatic analyses used a pipeline based on NextGENe® software and in silico tools for variant interpretation.
Findings: Our AmpliSeq™ custom-made panel efficiently explored 96.58% of the targeted sequences. Based on in silico analysis, 11 potentially pathogenic missense variants were identified that were not previously associated with AF. These variants were located in genes involved in atrial tissue structural remodeling. Three patients were also carriers of potential variants in prevalent arrhythmia-causing genes, usually associated with AF. Most of the variants were found in patients with atrial dilatation (n=9, 82 %).
Conclusion & Significance: This NGS approach was a sensitive and specific method that identified 11 potentially pathogenic variants, which are likely to play roles in the predisposition to left atrial myopathy. Functional studies are needed to confirm their pathogenicity.
- Video Presentation
Location: Amphi Theatre
Session Introduction
Vladimir Ermoshkin
Russian New University, Russia
Title: New theory of cardiovascular diseases
Time : 12:10-12:25

Biography:
Vladimir Ermoshkin completed his Graduation in Physics department at Moscow State University in 1978. He has worked at Russian New University (RosNOU) as Physicist. He has published 10 articles on Cardiology in prominent magazines (Russian and English).
Abstract:
Goal: An attempt to study the mechanism of metabolic syndrome.
Methods: Information search in the literature, participate in conferences, discussions with Russian leading cardiologists.
Results: Metabolic syndrome (MetS) is defined by a constellation of interconnected physiological, biochemical, clinical, and metabolic factors that directly increases the risk of cardiovascular disease and all cause mortality. Visceral adiposity, atherogenic dyslipidemia, endothelial dysfunction, genetic susceptibility, elevated blood pressure, hypercoagulable state, insulin resistance and chronic stress are the several factors, which constitute the syndrome. In my opinion, the researchers forgot to take into consideration a physical factor in the development of the metabolic syndrome. It is precisely the factor of gravity of the Earth which influence in the absence of regular physical exertion on the muscles of the lower half of the body, insufficiency of respiratory loads on the lungs and, most importantly, on the diaphragm. Previously, it was justified that large arteriovenous anastomoses (AVA) can be opened in a person under stress, high blood pressure (HBP), sedentary lifestyle and excessive nutrition. Increased pressure in the vena cava can lead to mechanically induced arrhythmias. The opening and closing of the AVA is characterized by jumps in the blood pressure as follows: first a sharp drop, then a smooth rise in 2-5 seconds. But the main factor leading to MetS is a constant useless leakage of arterial blood, an increase in the volume and pressure of venous blood, stagnation of blood in the depot. Frequent increases in venous pressure over time can lead to damage to venous valves, a lack of a pressure gradient between arterioles and venules in some organs. This deficiency in the erectile man due to gravity, especially at the initial stage, occurs mostly in the pelvic area and in the legs. It leads to stagnations, edemas, varicose. In response to such circulatory disturbances, blood contamination and violations of lymph movement, the body begins unsuccessful global neuro-humoral adjustments, but the situation most often does not improve, but worsens. Over time, MetS results in comorbidity of the disease and death from any of the causes associated with CVD.
Conclusions: Let’s consider that the proposed New Theory is still a hypothesis or an open problem. It is necessary to conduct a number of experiments, including with artificial AVA, for a data set to confirm or refute the new MetS hypothesis. If the proposed hypothesis proves to be correct, then the prevention and treatment of CVD can take a different path of development.
- Young Researchers Forum
Location: Amphi Theatre

Chair
Guy Hugues Fontaine
Universite Pierre et Marie Curie & La Salpetriere Hospital, France
Session Introduction
Manjit K Bhandal
Central Michigan University, USA
Title: Pulmonary artery intimal sarcoma: A review of the literature and case report
Time : 13:25-13:45

Biography:
Manjit K Bhandal is a second year MD student at Central Michigan University College of Medicine. Her primary interest in medicine is Cardiology in which she has several years of pre-clinical experience and is now conducting several studies in various aspects of the field. These studies include the present cardio-oncology study, outcomes of femoral artery catheterization in patients with US versus palpation techniques, as well as studying the outcomes of diabetic heart failure patients implanted with CardioMEMS.
Abstract:
Statement of the Problem: Pulmonary artery intimal sarcoma (PAIS) is a rare, aggressive tumor often diagnosed at autopsy. Presentation often involves the main pulmonary arteries and pulmonary valves with resultant pulmonary embolism and chronic thromboembolic pulmonary hypertension leading to the misdiagnosis of pulmonary embolic disease. Due to the paucity of data on the clinicopathologic features of disease in PAIS, the aim of this study was to combine a clinical case report with comprehensive review of literature with meta-analysis to increase awareness and facilitate clinical recognition of PAIS.
Methods: Clinical information was collected regarding tumor site, size, location, extension, patient presentation signs and symptoms, imaging data, disease recurrence, distant metastasis, and overall survival. Progression-free survival, distant-metastasis free survival, and disease-specific survival curves and estimates were calculated using the Kaplan-Meier method with univariate and multivariate analyses of prognostic variables calculated using Cox proportional hazards model.
Results: Kaplan-Meier survival plots did not indicate statistically significant correlations between mean survival and tumor location; however, metastasis and tumor recurrence showed statistical significance in correlation with mean survival time (P=0.21, P=0.31 respectively). Chi-square values indicated tumor location in the pulmonary valve and aorta were significant factors in mean survival time (P=0.004, P=0.23 respectively), as well as metastasis and tumor recurrence (P=0.003, P=0.001 respectively). The clinical case is of a 53-year-old woman with recurrent pulmonary emboli, claudication of legs, dyspnea and hemoptysis whom was later discovered to have a large (12.0x6.5x5.0 cm) intravascular lung pulmonary artery intimal sarcoma with satellite pulmonary metastases. Tumor cells showed immunohistochemical phenotypic expression of MDM2 and fluorescence in situ hybridization amplification of MDM2.
Conclusion & Significance: PAIS is a rare tumor type, clinicians treating patients for suspected PE that is refractory to anti-coagulant or thrombolysis therapy should have a high level of clinical suspicion for PAIS to improve outcomes.
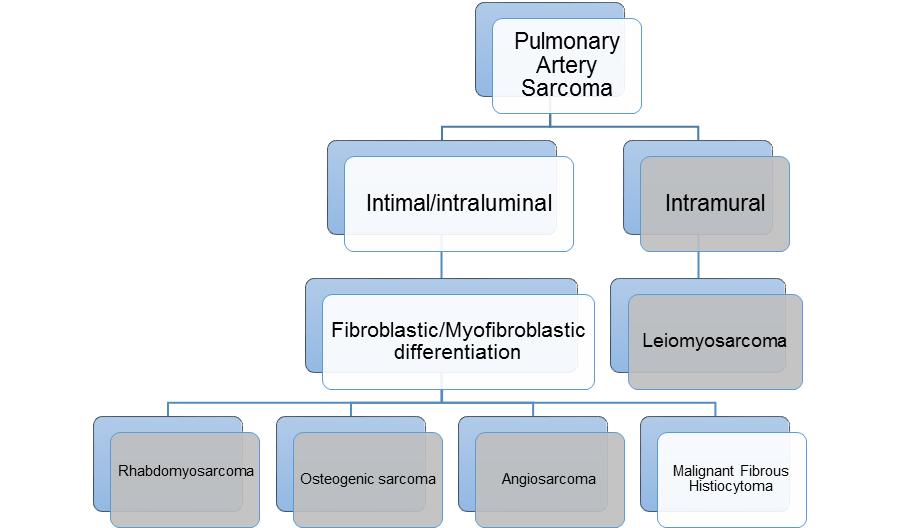
Figure 1: PAS is subdivided into intimal and intramural sarcomas. Intimal sarcomas are further classified as fibroblastic/myofibroblastic differentiation with several
different subtypes. The four most common are listed here. In this paper, we focus on malignant fibrous histiocytomas, also referred to as high grade spindle cell
sarcoma, or undifferentiated pleomorphic sarcoma (UPS).
References:
- Chen D, Zhu G, Wang D, Zhang Z, Fang W, Qu Z. Clinicopathological and immunohistochemical features of pulmonary artery sarcoma: A report of three cases and review of the literature. Oncol Lett. 2016;11(4):2820-2826.
- Chen X, Ren S, Li A, Zhou C. A case report of chemo-sensitive intimal pulmonary artery sarcoma. Cell Biochem Biophys. 2014;68(1):153-157.
- Dornas AP, Campos FT, Rezende CJ, Ribeiro CA, Amaral NF, Correa Rde A. Intimal sarcoma of the pulmonary artery: a differential diagnosis of chronic pulmonary thromboembolism. J Bras Pneumol. 2009;35(8):814-818.
- Fukuda W, Morohashi S, Fukuda I. Intimal sarcoma of the pulmonary artery--diagnostic challenge. Acta Cardiol. 2011;66(4):539-541.
- Kerr KM. Pulmonary artery sarcoma masquerading as chronic thromboembolic pulmonary hypertension. Nat Clin Pract Cardiovasc Med. 2005;2(2):108-112; quiz 113.
Amjed Eljaili
Betsi Cadwaladr University Health Board, UK
Title: Spontaneous coronary artery dissection (SCAD): Over view summary and literature review
Time : 13:45-14:05

Biography:
Amjed Eljaili, MBBS October 2010, University of Al-Zaiem Al-Azhari, Sudan, currently practicing in UK , Wales deanery , foundation year-2 trainee, BCUHB, emergency department. He attended several academic meetings, regionally and nationally. He has participated in various national work-shops, congress. participation and membership with British institute of Radiology, UK.
Abstract:
Spontaneous coronary artery dissection is rare cause of acute coronary syndrome in young female in reproductive period, the mechanism is completely different from common causes of coronary artery atherosclerotic disease. It has been reported that there is a significant link with underline blood vessels disease like fibromuscular dysplasia which is rare condition affect all arteries in the body, most common affected arteries are, renal and carotid artery which characterized by thickening of arterial wall leading to stenosis. Majority of patient affected were found to be female with median age between 20 to 60. The risk increased significantly during pregnancy between 5 to 18%, this ia can be 6 weeks per-partum and post-partum but up to 18 months also reported. Extreme emotional stress and physical exercise like heavy lifting and valsalva type of activity participating in the cause of SCADAS as well. Connective tissue disease like marfan synfrom, Ehler-denlos danols syndrome, systemic lupus erytrpmtpus polyarteritis nodpsa and inflammatory bowels disease can be participator factor for SCAD. The diagnosis of SCAD is a challenge and in most cases establishment of SCAD diagnosis has to be at time of coronary angiogram, intravascular ultrasound and OCT (optical coherence) tomography and IVUS intravascular ultrasound, according to coronary angiogram findings SCAD divided into three types. The management of SCAD in majority of the patients is conservative in form of aspirin , heparin, beta-blocker and ACE inhibitor along with clopidogrel in some patients, however revascularization by PCI and CABG depending on certain specific criteria. Overall long-term prognosis of SCADA is excellent but there is high risk of recurrence, interestingly recurrence in most cases involves a new coronary artery segment therefore patient with SCAD should always be counselled about the risk of recurrence of this condition.
Christina Meilani Susanto
Airlangga University, Indonesia
Title: Peripartum cardiomyopathy and its relationship with preeclampsia
Time : 14:05-14:25

Biography:
Abstract:
Causes of Maternal Mortality Rate (MMR) in Indonesia were having changes of trend. In the last three years, cardiac disease has become the second most cause of MMR after preeclampsia in our tertiary hospital. Peripartum Cardiomyopathy (PPCM) is one of cardiac disease that emerges in the last month of pregnancy or within five months of delivery in healthy women, without previous identifiable heart disease. The etiology remains unknown, but preeclampsia has been described to be a potential risk factor in the pathogenesis of the disease. Although there has been no study concerning the incidence of PPCM in Indonesia, it is well known that preeclampsia is still becoming a major issue of MMR in Indonesia. Location of study was at Dr Soetomo Hospital Surabaya, Indonesia. Data was obtained from medical record of 2843 patients within 2014-2015, divided into two groups, 19 patients with PPCM in a case group, and 2824 patients in control group. Peripartum cardiomyopathy patients had a mean age 32.21±6.83 years, whereas the mean age of control group was 29.26±6.45 (p=0.04). The incidence of PPCM in our study was quite high, about 1 per 166 live births. It was estimated that 52.63% cases were diagnosed antepartum, whereas 47.37% cases were diagnosed postpartum, with the mean ejection fraction 36.63±7.23%. It was a surprising result revealed, estimated 84.2% PPCM cases were also complicating with preeclampsia, and showing a significant difference between these two groups (p<0.05). Earlier onset of preeclampsia in our study described an earlier onset of PPCM as well, and about 81.8% babies born from PPCM mother were growth restriction babies. The mortality rate of the mother during hospitalization in our study is 15.7%. Although diagnosis of PPCM is still an exclusion diagnosis, we have to pay more attention to pregnant women complicating with preeclampsia, since preeclampsia can increase the risk of PPCM.
References:
- Bello N, Rendon I, Arany Z. (2013). The relationship between pre-eclampsia and peripartum cardiomyopathy. J Am Coll Cardio; 62:1715-23
- Elkayam U. (2012). Clinical characteristics of peripartum cardiomyopathy in the United States: diagnosis, prognosis, and management. J Am Coll Cardiol;58:659–70
- Elkayam U. Akhter M. (2005). Pregnancy-associated cardiomyopathy clinical characteristics and a comparison between early and late presentation. Circulation;111:2050-2055
- Kamiya C. Kitakaze M. (2010). Different characteristics of peripartum cardiomyopathy between patients complicated with and without hypertensive disorders. Circ J; 75:1975-1981
- Sliwa K. Kleiner D. (2010). Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group of peripartum cardiomyopathy. European J of Heart Failure;12:767-778
Dibya Arfianda
Airlangga University, Indonesia
Title: Pregnancy outcomes in rheumatic heart disease
Time : 14:25-14:45

Biography:
Dibya Arfianda is a Resident of Obstetrics and Gynecology at Airlangga University, Indonesia.
Abstract:
Pregnant women with acquired heart disease could lead to fatal outcome if not properly managed. Rheumatic fever is a secondary to rheumatic heart disease that cause defect at heart valves and the most common is mitral stenosis. In first trimester of pregnancy, the cardiac output is increasing at about 50% due to hormonal change that has effect to vascular and elevated plasma in blood. These changes will directly alter to mother condition with valve defect and require prompt management. A comprehensive multidisciplinary approach is also needed in managing morbidity and mortality of RHD in pregnancy. A retrospective analysis study of pregnancies with RHD was conducted from January until December 2015 at RSUD Dr. Soetomo Surabaya, Indonesia. We have collected 1.289 medical records. Total 21 (3.2%) cases were patients with acquired heart disease. 17 (81%) cases were patients with prime gravida. More than half cases found were preterm pregnancy. Multiple valve disease which involved the mitral stenosis and other valves were the usual finding in these cases. Complications such as pulmonary hypertension, lung edema, heart failure usually found in our cases. Cesarean section was the preferred mode of delivery from all patients. Two patients died after delivering their baby (10%). We also did PTMC in two (9.5%) patients during pregnancy. Pregnancy with RHD has a great link and contribution to the increment of maternal morbidity and mortality.
References:
- Chamaidi, A., Gatzoulis, M. (2006). Heart Disease and Pregnancy. Hellenic J Cardiol 47: 275-291
- Gumilar, K.E., Aditiawarman, Lefi, A. (2015). Maternal outcome on pregnancy with rheumatic heart disease.
- Madazli, R., Sal, V., Cift, T., Guralp, O., Goymen, A. (2010). Pregnancy outcomes in women with heart disease. Arch Gynecol obstet 281: 29-34
- Pratibha, D., Devineni, K., Vemuri, U., Namani, G. (2007). Pregnancy outcome in chronic rheumatic heart disease. Journal of Obst & Gyn: 59(3),pp11-21
- Silversides, C.K., Colman, J.M. (2007). Heart Disease in Pregnancy 2nd Edition. Chap-2: Physiological changes in pregnancy. Masachusetts: Blackwell publishing pp79-95.
