Day 2 :
Keynote Forum
Mark Caulfield
William Harvey Research Institute & Queen Mary University of London, UK
Keynote: Advances in the genomics of blood pressure: Time for translation
Time : 09:05-09:40

Biography:
Professor Mark Caulfield graduated in medicine in 1984 and trained in Clinical Pharmacology at St Bartholomew’s Hospital where he developed a major programme in genetics of blood pressure regulation. In 2002 he became Co-Director of the William Harvey Research Institute at Queen Mary University of London which he grew from 140 to 530 clinicians and scientists and a major worldwide pharmacological centre focused on cardiovascular, inflammation and endocrine research. He was President of the British Hypertension Society and served on the council of the European Society of Hypertension. In 2013 he became an NIHR Senior Investigator and Chief Scientist for the 100,000 Genomes Project.
Abstract:
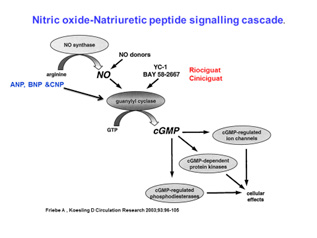
Statement of the problem: Hypertension is the commonest cardiovascular worldwide with an anticipated 1.5 billion people with high blood pressure by 2025. It arises from a complex interplay between genes and lifestyle. From family studies between 30-50% of the heritability of blood pressure is due genetic influences or gene plus lifestyle. Approximately 8-12% of hypertensives cannot tolerate or are resistant to current therapies. Understanding the genes underpinning blood pressure could identify new biological pathways for innovative therapeutics. In genome wide studies of blood pressure now expanded to more than 1000 gene loci for blood pressure discovered and validated in over 1 million people. Many of these loci identify new biological pathways and some repurposing opportunities for existing therapies used for other disorders. A genetic risk score of all aggregate variants at 1000 loci suggested that in the over 50 year olds these loci cause a potential 10 mm Hg rise in blood pressure. This prompts the question is it tie to translate these findings into the clinic. First a targeted gene chip could identify those at risk in early life and enable lifestyle measures such as exercise a diet rich in fruit and vegetables, maintenance of an ideal body weight and reduced alcohol intake. In addition in mechanistic studies we and others have identified potential therapies acting on the nitric oxide-natriuretic peptide pathway including beetroot juice and c-natriuretic peptide mimetics. We can also now deploy next generation sequencing techniques to diagnose the cause of rare syndromic forms of hypertension and the impact of that will be explored.
Recent Publications
1. Warren HR, Evangelou E, Cabrera CP, Gao H, Ren M, Mifsud B, and multiple co-authors then, Caulfield M., Elliott P. Genome-wide association analysis identifies novel blood pressure loci and offers biological insights into cardiovascular risk. Nat Genet. 2017 Mar; 49(3):403-415. doi: 10.1038/ng.3768.
2. Georg B. Ehret then multiple co-authors then Mark J. Caulfield, Toby Johnson. Genetic variants from novel pathways influence blood pressure and cardiovascular disease risk. Nature 2011; 478(7367):103-9.
3. Louise V Wain, then multiple authors then Mark J Caulfield, Dabeeru C Rao, Martin D Tobin, Paul Elliott, Cornelia M van Duijn. Genome-wide association study identifies six new loci influencing pulse pressure and mean arterial pressure. Nature Genetics 2011 Sep 11; 43(10):1005-11.
4. Newton-Cheh C, then 152 co-authors then Elliott P, Abecasis GR, Caulfield M, Munroe PB. Genome-wide association study identifies eight loci associated with blood pressure. Nature Genetics 2009 May 10. [Epub ahead of print] PubMed PMID: 19430483.
Keynote Forum
Rohit Arora
Professor of Medicine, Chicago Medical School, USA
Keynote: Effect of smoking on coronary microvasculature in hospitalized chest pain patients
Time : 09:40-10:15

Biography:
Dr. Rohit Arora is currently Professor of Medicine and Professor of Physiology and Biophysics, Chicago Medical School, Chicago, Illinois where he is also Chairman of Cardiology and Vice- Chairman of Medicine, Department of Medicine. He is also Chairman of Medicine and Chief of Cardiology at the Principal Teaching Hospital at the James Lovell FHCC, North Chicago IL. Previously, he was Chief of Cardiology at UMDNJ and Director of Interventional Cardiology and Catheterization Laboratory, New Jersey, and Director of Critical Cardiology, and Director of Cardiac Care Units at Columbia Presbyterian Medical Center, at Columbia University in New York. Dr. Arora’s residency training was at the Mount Sinai School of Medicine, New York, with a fellowship at Mount Sinai Medical Centre in New York, Nuclear cardiology fellowship also at Mount Sinai, Interventional fellowship at the Cleveland Clinic Foundation, Cleveland, Ohio. He does lectureship in thrombosis and vascular disease at Montefiore Medical Centre/Albert Einstein School of Medicine, NY. Dr Arora’s research interests include thrombosis, refractory angina, EECP, lipids, vascular biology of the endothelium, interventional, and preventive cardiology. He has authored or co-authored more than five hundred papers and abstracts, and is the recipient of numerous awards & honors. Dr Arora is on the editorial board of numerous medical journals, and was the editor of Heart International. He has co-authored a textbook on Clinical Autonomic Dysfunction, available on Amazon, by Springer. He is nominated to the FDA device panel for devise and radiological devices. He has performed pioneering studies in refractory angina and Enhanced External Counter-pulsation.
Abstract:
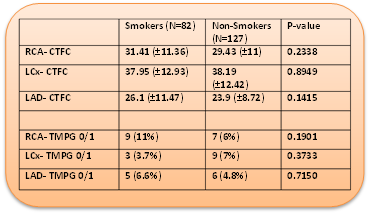
Background: Multiple studies demonstrate increased Thrombosis in Myocardial Infarction (TIMI) frame count (cTFC) among tobacco smokers (TS) even in the absence of epicardial coronary artery disease (CAD), suggestive of coronary microvascular dysfunction (MD). Among those patients who present with chest pain and a positive stress test, we hypothesize that the extent of MD is larger among TS when compared to non-smokers (NS).
Method: In this retrospective study, patients who underwent coronary angiogram for chest pain with a positive stress test were grouped into TS and NS. Among these, those who were free of a significant CAD, vasospasm or recent myocardial infarction were randomly chosen: 82 TS and 127 NS. Presence of coronary MD was assessed using cTFC and TIMI perfusion grade (TMPG).
Results: At baseline, TS were significantly younger compared to NS (mean age in years 50.2 vs 58.56, p<0.0001) with significantly more females in the NS group. The cTFC and TMPG for left anterior descending, left circumflex and right coronary arteries though significantly higher in both groups, when compared to published normals, there was no significant difference observed. Additional sub-group analysis for gender and age (<50 years and ≥50 years) also did not demonstrate any significant differences. Furthermore, among patients with no history of hypertension, diabetes mellitus and hyperlipidemia, no significant differences were observed between the two groups.
Conclusion: Increased cTFC in both the groups indicates increased coronary microvascular resistance suggesting MD, which may be the reason for a positive stress test. This study demonstrates that among patients presenting with chest pain and a positive stress test, in the absence of significant epicardial CAD, tobacco smoking does not further increase MD.
Recent Publications:
- Crea F, Camici PG, Bairey Merz CN.Coronary microvascular dysfunction: an update.Eur Heart J. 2014 May;35(17):1101-11. doi: 10.1093/eurheartj/eht513.
- The TIMI Study Group. The Thrombolysis In Myocardial Infarction (TIMI) trial. N Engl J Med. 1985;31:932–936.
- Gibson CM, Cannon CP, Murphy SA, et al. Relationship of TIMI Myocardial Perfusion Grade to Mortality After Administration of Thrombolytic Drugs. Circulation. 2000;101:125.
- Gibson CM, Cannon CP, Daley WL, et al. TIMI Frame Count. Circulation. 1996;93:879-888.
- Erbay, Ali Riza et al. “Documentation of slow coronary flow by the thrombolysis in myocardial infarction frame count in habitual smokers with angiographically normal coronary arteries.” Heart and Vessels 19 (2004): 271-274.
Keynote Forum
Antonis A. Armoundas
Assistant Professor, Harvard Medical School, USA
Keynote: Real-time detection and suppression of repolarization alternans as antiarrhythmic therapy
Time : 09:40-10:15

Biography:
Antonis A Armoundas completed his BS in Electrical Engineering from National Technical University of Athens, Athens, Greece, in 1991 and MS in Biomedical Engineering from Boston University, Boston, MA, in 1994. He received PhD in Nuclear Engineering, from the Massachusetts Institute of Technology (MIT), in 1999. He was an American Heart Association sponsored Post-doctoral Fellow at the Division of Molecular Cardiobiology and the Department of Biomedical Engineering at Johns Hopkins University. Now, he is a National Institute of Health supported Principal Investigator at Massachusetts General Hospital and an Assistant Professor at Harvard Medical School, while he maintains an appointment at M.I.T. He has authored more than 80 high-impact peer-reviewed journal articles and book chapters, and he also holds six patents. His
research interests include “Biomedical signal processing, forward and inverse problem solutions, and cellular electrophysiology methods”.
Abstract:
Background: This study investigates the spatio-temporal variability of intracardiac repolarization alternans (RA) and its relationship to arrhythmia susceptibility in a swine acute myocardial ischemia (MI) model.
Methods & Results: We developed a real-time multi-channel repolarization signal acquisition, display and analysis system to record electrocardiographic signals from catheters in the right ventricle, coronary sinus and left ventricle prior to and following circumflex coronary artery balloon occlusion. We found that RA is detectable within 4 minutes following the onset ischemia, and is most prominently seen during the first half of the repolarization interval. We developed a novel, clinically-applicable intracardiac lead system based on a triangular arrangement of leads spanning the right ventricular (RV) and coronary sinus (CS) catheters which provided the highest sensitivity for intracardiac RA detection when compared to any other far-field bipolar sensing configurations (p < 0.0001). The magnitude of RA was used to adjust pacing stimuli delivered during the absolute refractory period (ARP) aimed to reduce RA. We found that the pacing pulse polarity and the phase polarity are sufficient parameters to suppress RA. To calibrate the pacing stimuli, we estimated the required charge to induce one μV [one unit] change in the alternans voltage [and Kscore] on CS and LV leads as 0.05 ± 0.025 [0.32 ± 0.29] and 0.06 ± 0.033 [0.33 ± 0.37] μC, respectively. Using this approach, we demonstrated the ability to suppress spontaneous RA following acute MI. Overall, pacing during the ARP resulted in a significant decrease in alternans
voltage and Kscore and reduced arrhythmia susceptibility (p<0.01).
Conclusion: RA can be reliably detected through a novel triangular RV-CS lead configuration. Electrical stimulation during the ARP can be used to suppress RA, in vivo. Our findings may have important implications in developing methods to prevent the onset of ventricular arrhythmias.
Recent Publications
1. Merchant FM and Armoundas A A. Role of substrate and triggers in the genesis of cardiac alternans, from the myocyte to the whole heart: Implications for therapy. Circulation. 2012;125:539-549.
2. Sayadi O, Puppala D, Ishaque N, Doddamani R, Merchant F M, Barrett C, Singh J P, Heist E K, Mela T, Martinez J P, Laguna P and Armoundas A A. A novel method to capture the onset of dynamic electrocardiographic ischemic changes and its implications to arrhythmia susceptibility. J Am Heart Assoc. 2014;3.
3. Sayadi O, Merchant F M, Puppala D, Mela T, Singh J P, Heist E K, Owen C and Armoundas A A. A novel method for determining the phase of t-wave alternans: Diagnostic and therapeutic implications. Circ Arrhythm Electrophysiol. 2013;6:818-826.
4. Merchant F M, Sayadi O, Moazzami K, Puppala D and Armoundas A A. T-wave alternans as an arrhythmic risk stratifier: State of the art. Curr Cardiol Rep. 2013;15:398.
5. Merchant F M, Sayadi O, Puppala D, Moazzami K, Heller V and Armoundas A A. A translational approach to probe the proarrhythmic potential of cardiac alternans: A reversible overture to arrhythmogenesis? Am J Physiol Heart Circ Physiol. 2014;306:H465-474.
- Cardiac Surgery | Cardiac Nursing | Cardio-Oncology | Pediatric & Geriatric Cardiology | Interventional Cardiology | Hypertension
Location: Gatwick Hall

Chair
Antonis A Armoundas
Harvard Medical School, USA

Co-Chair
Athos Capuani
Private Organization Carrara, Italy
Session Introduction
Guo-Wei He
TEDA International Cardiovascular Hospital, China
Title: Multi-omics studies in cardiovascular diseases: Our experience
Time : 10:15-10:40

Biography:
Professor Guo-Wei He, MD, PhD ((Monash), DSc (Monash) is Vice President and Chief (Academic) and Senior Surgeon of Department of Cardiovascular Surgery, as well as Director, Center for Basic Medical Research, TEDA International Cardiovascular Hospital (from October, 2007-), Chinese Academy of Medical Sciences & Peking Union Medical College, Tianjin, China. Professor He currently also holds Clinical Professor of Surgery, Department of Surgery, Oregon Health and Science University, Portland, OR, U.S.A. and Chair Professor, Zhejiang University as well as Hangzhou Normal University, China. Previously, Professor He was Chair Professor of Cardiothoracic Surgery, Department of Surgery, University of Hong Kong & Honorary Consultant Cardiac Surgeon, The Grantham Hospital, Hospital Authority, Hong Kong and then Research Professor of Surgery & Director, Cardiovascular Surgical Research Laboratory, Department of Surgery, The Chinese University of Hong Kong, Hong Kong and Professor of Surgery at Nankai University. He was also Director, Cardiovascular Research, Starr Academic Center, Providence Heart Institute, Portland OR, U.S.A. Professor He is (or was) a member of editorial board for more than 20 international journals including The Annals of Thoracic Surgery (U.S.A.), World Journal of Surgery (U.S.A.) , and The Heart Surgery Forum (U.S.A.). He received a number of science award including First Prize, 2012 Tianjin (China) Natural Science Award. He is awardee of a number of Research Grants from Research Grants Council, Hong Kong, Am. Heart Assoc., St. Vincent Medical Foundation, U.S.A. and more recently from National Science Foundation & The Ministry of Science & Technology, China. Professor He has contributed in a number of books. In addition, as the sole editor, he has published a book entitled: Arterial Grafts for Coronary Artery Bypass Grafting Surgery (Springer-Verlarg); this book has been published in two editions now with an additional edition in Chinese. Professor He has had 321 publications indexed by SCI (Science Citation Index, U.S.A.) and 202 full papers including editorials indexed by “Pub Med” including multiple papers in “Circulation”.
Abstract:
In the “Precision Medicine” era, integration of multiple ‘omics’ technologies will allow us to gain a more complete picture of the constituents and functions of diseases and provide far richer information for predictive modelling of phenotypes.
The multiple ‘omics’ technologies largely refer to high-throughput technologies that have revolutionized medical research. These technologies allow integrative studies at genomic, epigenomic, transcriptomic, proteomic, and metabolomic levels, etc. In cardiovascular diseases, genomics, epigenomics, transcriptomics, proteomics, and metabolomics are particularly important in understanding the mechanisms of the disease. Multi-omics offers the opportunity to understand the flow of information that underlies cardiovascular diseases better than the studies at a single omics level.
We have been using these multi-omics technologies in coronary artery disease, heart valvular diseases, and congenital heart diseases. With the multi-omics studies, we now have deeper understanding of the complexity in mechanism(s) of these diseases. This lecture will detail some of our studies as well as views on the prospects in this area.
Athos Capuani
Private Organization Carrara, Italy
Title: New perspectives in pediatric cardiology and cardiac surgery
Time : 10:55-11:20

Biography:
Athos Capuani is a Cardiothoracic Surgeon with a long working experience in acquired and congenital heart diseases. For the recent years he is very interested in fetal life. The main area of investigation is the embryology-morphology of CHD and the links with genetic and epigenetic disorders. He found an anatomical common denominator in the most complex malformations: The Trabecula Septomarginalis sequential malrotation. He thinks that many complex CHD could be addressed during pregnancy on the light of this model and the modern molecular biology what he refers as Molecular Cardiac Surgery.
Abstract:
Statement of the Problem: The classical congenital heart surgery in complex malformations still carries high risk and poor long term outcome despite the advances marked over the 20th century.
Hypothesis: A very early diagnosis and non invasive treatment during pregnancy on the light of the modern molecular biology would strongly affect the medical and surgical history of Congenital Heart Diseases (CHD).
Methodology: We reconsidered the embryogenesis and the morphology of the most severe CHD.
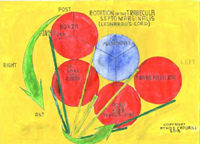
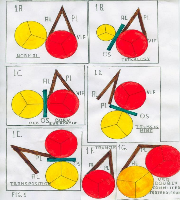
Findings: We found a common anatomical denominator in all morphological settings: the Trabecula Septomarginalis sequential malrotation counterclockwise apex-base axis (TSM, Leonardo’s cord). The TSM is composed in the normal heart by an Anterior Limb AL committed to the Outlet Septum and by a Posterior Limb PL committed to the inner curvature. Fig.1. TSM (brown) and Outlet Septum (green) rotation in sequential phenotypes from normal to Transposition of Great arteries. Fig.2. TSM rotation seen from the apex: PL green, AL Yellow. The TSM rotating follows the development of the right ventricle and is always traceable in the classical V shape or variants.
Conclusions:
- The TSM sequential malrotation is proposed as a model for new investigations and treatments during pregnancy.
- Each malformed cardiac phenotype has a specific molecular profile which can be identified by the Next Generation Sequencing analysis (NGS) and edited by the CRISPR-cas9 technique what we refer as NGS Molecular Cardiac Surgery.
Recent Publications:
- Capuani A (2017) New Perspectives in Cardiac Surgery: The Virtual Ventricle and the Molecular Cardiac Surgery. Proceedings of 7th World Congress of Pediatric Cardiology and Cardiac Surgery. Barcelona 2017,P2271:726-727. www.wcpccs2017.org.
- Capuani A (2016) Targeting exome sequences in congenital heart diseases: are we there yet? Proceedings of the XXXI Congress of the International Academy of Pathology and 28th Congress of the European Society of Pathology. Cologne 2016, Virchows Archiv 2016; 469(Suppl1):S1-S346 E-PS-02-003,pp s242.
- Capuani A (2015) Potential treatment of congenital heart malformations during cardiac morphogenesis. Proceedings of the 27th European Congress of Pathology. Belgrade 2015, Virchows Archiv 2015;467(Suppl1):S1-S279 PS05-005,pp s97.
- Capuani A (2014) The trabecula septomarginalis (Leonardo’s cord) in abnormal ventriculo-arterial connections. J Cardiothorac Surg 2014;9:71-81.
Alexander Manché
Mater Dei Hospital, Malta
Title: Long-term relative survival study after surgical aortic valve replacement in patients with intermediate risk
Time : 11:20-11:45

Biography:
Alexander Manché is the Chairman of the Cardiothoracic Surgery at Mater Dei Hospital, Malta. He qualified at Westminster Medical School, London in 1979 and spent 18 years in the UK and the US, including 2 years of research at the Rayne Institute. He returned to Malta in 1995 and set up the Cardiothoracic Unit, which offers a comprehensive adult service including surgery for ischaemic and valvular heart disease, thoracic vascular conditions, heart transplantation, vascular access as well as lung disease. His journal publications and presentations at scientific meetings number over two hundred. He has a special interest in the epidemiology of aortic valve surgery.
Abstract:
The indications for Transcatheter Aortic Valve Implantation (TAVI) are evolving. The original indication, in patients with unacceptably high risk for surgery, was expanded to include high-risk patients also eligible for surgery. TAVI is now being offered to intermediate-risk patients without available long-term data. Surgery in these patients offers excellent results, both in the short and long term.
Surgical aortic valve replacement, with or without concomitant coronary revascularisation, can achieve a normal life expectancy in intermediate-risk patients aged 68 or older. We present a 20-year relative survival study, comparing patients’ outcomes with that of normal controls derived from the National Statistics database. The study also correlated long-term survival with patient-related, procedure-related and post-operative complication-related factors.
Surgical AVR for severe aortic stenosis in intermediate-risk patients yields excellent long-term survival. The decision to offer TAVI to these patients should factor in the known long-term results of surgery.
Recent Publications:
- Long-term outcomes after surgical aortic valve replacement. A Manché. Cardiothoracic Department, Mater Dei Hospital, Malta. J Clin Exp Cardiolog 2017, 8:9(Suppl): 31. doi: 10.4172/2155-9880-C1-077.
- TAVI : Trans-Apical and trans-Aortic approaches. A Manché. Invited speaker in symposium on The TAVI Experience in Malta. Drugsales Ltd, in conjunction with Edwards Life Sciences. October 2011.
- Initial TAVI experience in Malta. A Manché, A Cassar, A Fenech. Oral presentation, 8th Maltese Medical School conference, Malta, November 2012.
- Early surgical intervention in aortic valve disease. A Manché. Oral presentation, 5th Annual meeting of the Maltese Cardiac Society, Malta, October 2014.
- Should patients with asymptomatic severe aortic stenosis be referred for surgery? A Manché. Oral presentation, International Congress of Cardiology, Malta, March 2015.
- Is valve size more important than patient-prosthesis mismatch in long-term survival after aortic valve replacement? A Manché, L Camilleri. Malta Medical Journal 2015; 27:Suppl. 95 Abstract P3.06.
- Long-term survival after aortic valve replacement: A twenty-year relative survival study. A Manché, L Camilleri, D Gauci. Malta Medical Journal 2015; 27:Suppl. 64 Abstract OP6.18.
- Does aortic valve replacement restore normal life expectancy? a twenty-year relative survival study. A Manché, L Camilleri, D Gauci. International Cardiovascular Forum Journal 2016;6:3-10.
- At what age does aortic valve replacement restore life expectancy? A Manché, L Camilleri. SCTS Conference News. The official newspaper of the SCTS Annual Meeting and Cardiothoracic Forum 2016. page 30.
- The myths and challenges of patient-prosthesis mismatch. A Manché. Oral presentation 7th Annual meeting of the Maltese Cardiac Society, Malta, October 2016.
- The impact of age in prosthesis-patient mismatch on long-term survival after aortic valve replacement: in-vitro versus in-vivo values. A Manché, A Casha, L Camilleri. Journal of Advances in Medical and Pharmaceutical Sciences 2016;9:1-8 JAMPS.28381 ISSN: 2394-1111.
Fabiola B Sozzi
Ospedale Maggiore Policlinico CÃ Granda, Italy
Title: Echocardiographic diagnosis of diastolic heart failure
Time : 11:45-12:10

Biography:
Fabiola Sozzi works as a staff cardiologist at the University Hospital Policlinico of Milan, Italy, with high-specialization nomination. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She gained a high expertise in echocardiography at the Thoraxcentre of Rotterdam (NL), where she defended the PhD thesis on stress cardiac imaging under the supervision of Professor J. Roelandt. She is Visiting Professor at the University of Milan where she leads several research projects and teaches at the Faculty of Medicine and School of Specialization of Cardiology. She is author of 70 papers published in indexed peer-reviewed international journals and reviewer of several medical international journals.
Abstract:
Chronic dyspnea is associated with a variety of diseases and is also a major symptom of heart failure (HF). The differential diagnosis of dyspnea is a daily routine in every cardiology practice. Approximately one-half of patients with HF have a preserved ejection fraction (HFpEF). Diagnosis of HFpEF is challenging and relies largely on demonstration of elevated cardiac filling pressures represented by the pulmonary capillary wedge pressure.
Healthy individuals with normal relaxation are able to increase the rate of myocardial relaxation when there is a need for increased diastolic filling. Faster relaxation allows the achievement of a lower minimal left ventricular (LV) diastolic pressure at a shorter time interval than in the resting state. Hence, increased LV filling can occur even with a shortened diastolic filling time. When myocardial relaxation is reduced in the resting state, it cannot be increased as much as necessary to meet the demands of exertion or stress. In this situation with abnormal myocardial relaxation, a reduced diastolic filling period and a lack of atrial contraction compromise LV filling substantially, causing the increase in left atrial and LV diastolic pressures (hence, decreased diastolic reserve).
Collectively, there is growing evidence that the diastolic stress test can provide important diagnostic findings that can be helpful in the management of patients presenting with dyspnea of an unclear etiology. Many patients present with exertional dyspnea and exercise intolerance, but have normal LV filling pressures at rest. In these patients, it is important to evaluate filling pressure with exercise. Exercise can be performed using a supine bicycle or treadmill protocol. Alterantively dobutamine can be used, though its vasodilator as well as inotrope effect determine a very different hemodynamic response compared to that of exercise. We need to record mitral inflow by pulsed Doppler echocardiography at the level of the mitral tips, mitral annular velocities by spectral Doppler echocardiography, and tricuspid regurgitation jet by continuous-wave Doppler at baseline and after the termination of exercise. Diastolic function parameters can be obtained after the assessment of regional wall motion abnormalities, especially when an exercise echocardiogram is performed for the evaluation of dyspnea. In patients with diastolic heart failure, left atrial pressure is increased, leading to an increase in mitral E velocity, whereas annular e’ velocity remains reduced given the limited preload effect on e’. Moreover, an increase in the pulmonary artery systolic pressure can be detected by the increase in peak velocity of the tricuspid regurgitation jet. On the other hand, in the absence of cardiac disease, e’ increases to a similar extent to the increase in mitral E velocity, and the normal E/e’ ratio essentially is unchanged with exercise. The concept of the diastolic stress test were introduced more than 10 years ago by Ha et al. Subsequently, exercise E/e’ ratio was validated against invasive measurements. Importantly, exercise septal E/e’ ratio was an important determinant of exercise capacity, and its decline with age was noted in a large series of patients referred for exercise echocardiography. Furthermore, a recent study showed the incremental prognostic value of exercise E/e’ ratio over clinical variables and exercise wall motion score index.
In conclusion, diastolic stress test has an interesting role in patients with heart failure and preserved ejection fraction that present symptoms during activity, normal ejection fraction and inconclusive diastolic function at rest.
Recent Publications:
- Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009; 10:165-193.
- Oh JK, Park SJ, Nagueh SF. Established and Novel Clinical Applications of Diastolic Function Assessment by Echocardiography. Circ Cardiovasc Imaging 2011;4:444-445.
- Ratanasit N, Karaketklang K, Chirakarnjanakorn S, Krittayaphong R, Jakrapanichakul D. Left atrial volume as an independent predictor of exercise capacity in patients with isolated diastolic dysfunction presented with exertional dyspnea. Cardiovascular Ultrasound 2014,12:19-26.
- Ha J, Oh J, Redfield M, Ujino K, Seward J, Tajik A. Triphasic mitral inflow velocity with middiastolic filling: clinical implications and associated echocardiographic findings. J Am Soc Echocardiogr. 2004;17: 428–431.
Helena Dominguez
Frederiksberg Hospital & University of Copenhagen, Denmark
Title: Systematic closure of the left atrium appendage during surgery: The LAACS and LAACS2 randomized studies
Time : 12:10-12:35

Biography:
Helena Domínguez, MD, PhD, is Consultant Cardiologist at the Hospital of Bispebjerg-Frederiksberg since 2014, and Associate Professor in the Institute of Biomedicine of the Health Faculty, University of Copenhagen. Her research covers translational science in two main areas: i) vascular function, with special focus on insulin resistance, and ii) use of eHealth technologies to improve patient management, with special focus on frail elderly, heart failure and atrial fibrillation. Teaching responsibilities: Lung and Heart Physiology, and Electrocardiography and Echocardiography exercises for medicine students. Postgraduate courses target PhD students within the area of vascular insulin resistance and methods to study vascular function.
Abstract:
Stroke from thombi formed in the left atrium appendage (LAA) is the most feared complication of atrial fibrillation (AF), and is preventable with anti-coagulant medicines. AF with onset the days after heart surgery is considered a phenomenon rather than a definite diagnosis, and anti-coagulation in not systematically recommended in current guidelines. We hypothesize that; closure of the LAA during surgery may protect the brain regardless of known AF.
Between 2010 and 2015 we included 205 patients, of whom 185 were randomized 185 to closure of the LAA with double suture, or control, and followed the patients for up to six year (mean 3,7 years). Investigations included brain MRI before the operation, at discharge after the operation and, at least six months after surgery, and findings of new silent brain infarctions (SBI) in clinical settings. 141 patients followed the protocol, of whom 14 (18%) reached primary events (stroke, TIA or silent infarctions) occurred in the control group vs. 4 (6%) in the LAACS group (hazard ratio 0.3; 95% CI: 0.1 – 1.0, p=0.05). In the total cohort, 163 (86.2%) had no history of AF, of whom 80 (49.1%) developed new-onset AF. Later AF occurred in 35 of those (43.8% recurrence) and, in six additional patients. The moderate number of patients in the LAACS trial does not allow to draw definite conclusions. Hence, we seek to further investigate our hypothesis in a larger trial (N 2000) with homogenous closure of the LAA with clips, and end-point of stroke/TIA.
Camelia Nicolae
Assistant Professor, Internal Medicine & Cardiology Department, Carol Davila University of Medicine and Pharmacy, Romania
Title: Ischemic stable coronary disease: Between guidelines and “real lifeâ€
Time : 12:35-13:00

Biography:
Camelia Nicolae, PhD is currently the Assistant Professor at Internal Medicine and Cardiology Department, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania. She has been working in the Coronary and Intensive Care Unit since graduation. In clinical activity, she was interested in diagnosis and treatment of acute coronary syndrome, acute cardiac failure and pulmonary thromboembolism. She had a special preoccupation about ventricular remodelling post-acute myocardial infarction, which was reflected in her doctoral thesis. After the publication of the latest cardiology guidelines about stable coronary ischemic disease, she developed a constant interest in the high incidence and prevalence of this pathology “in real life”. Dr. Nicolae is constantly searching diagnostic solutions for early identification of coronary ischemic disease in different subgroups of general population with high cardiovascular risk, that don’t have a detailed approach accordingly to current protocols. In her career, she sustained and published over 70 scientific papers and original studies and in the last three years public conferences were mainly focused on stable coronary ischemic disease.
Abstract:
Statement of the problem: The aim of the conference is to emphasize the difference between incidence, prevalence and mortality of stable coronary ischemic disease in “real life” and the data from the guidelines. In the light of current protocols, we diagnose and stratify the risk of stable coronary ischemic disease depending on gender, age and the presence of chest pain. This approach ignores a significant number of asymptomatic subjects who present one or more cardiovascular risk factors. Among this, diabetes mellitus and chronic kidney disease represents clinical equivalents of coronary ischemic disease as the guidelines specifies.
Theoretical orientation: According to a lot of clinical studies performed in UK and USA, the majority percent of sudden death is caused by ischemic heart disease. So, what are the reasons to exclude from diagnose and risk stratification the most vulnerable candidates? Messrs Bayes de Luna and Roberto Elosua proved in a remarkable study published in 2012, that the greatest numbers of sudden deaths, 300.000/ year are encountered in general population. The second most frequent sudden deaths, 250.000/year, are registered in the subgroup with risk factors in general population. In another study performed in USA and published in 2008, 80% of sudden deaths were caused by coronary ischemic disease. According to the most recent statistic data, the mortality decreases in ischemic heart disease, but its incidence is increasing.
Conclusion: Current guidelines mention that the avoidance of excessive costs for elaborated investigation represented a constant concern, but in “real life” coronary ischemic disease remains under- diagnosed and under- treated. Recommendations: every clinical physician must decide upon the most proper methods to diagnose coronary ischemic disease depending on the clinical data of the patient.
Recent Publications:
- Kee-Joon Choi,MD, Jae-Kwan Song, MD, You-Ho Kim, MD, Seong-Wook Park, MD, Seung-Jung Park, MD, Jung-Min Ahn, MD, Ki Hong Lee,MD, Sang-Yong Yoo, MD, Young-Rak Cho, MD, Jon Suh, MD, Eun-Seok Shin,MD, Jae-Hwan Lee, MD, Dong Il Shin, MD, Sung-Hwan Kim, MD, Sang Hong Baek,MD, Ki Bae Seung, MD, Chang WookNam,MD, Eun-SunJin,MD, Se-WhanLee,MD, Jun HyokOh,MD, JaeHyunJang, HyungWookPark,MD, Nam Sik Yoon,MD, Jeong Gwan Cho,MD, Cheol Hyun Lee, MD, Duk-Woo Park, MD, Soo-Jin Kang, MD, Seung-Whan Lee, MD, Jun Kim, MD, Young-Hak Kim, MD, Ki-Byung Nam, MD, CheolWhan Lee, MD, ( 2016), Prognosis of Variant Angina Manifesting as Aborted Sudden Cardiac Death, J Am Coll Cardiol;68:137–45.
- Wilkins E, Wilson L, Wickramasinghe K, Bhatnagar P, Leal J, Luengo-Fernandez R, Burns R, Rayner M, Townsend N (2017), European Cardiovascular Disease Statistics, European Heart Network.
- Antonio Bayes de Luna, Roberto Elosua, (2012), Sudden Death, Rev Esp Cardiol; 65:1039-1052.
- Jaskanwal D. Sara, MBChB; Mackram F. Eleid, MD; Rajiv Gulati, MD, PhD;and David R. Holmes Jr, MD, (2014), Sudden Cardiac Death From the Perspective ofCoronary Artery Disease,Mayo Clin Proc, 89(12):1685-1698.
- Sumeet S. Chugh, Kyndaron Reinier, Jonathan Jui, (2008), Epidemiology of sudden cardiac death: clinical and research implication, Prog Cardiovasc Dis, 51(3): 213-228.
- Workshop
Location: Gatwick Hall
Session Introduction
Sergio Mejia Viana
St. Bernard´s Hospital, Gibraltar
Title: Chemical, physical and emotional stressors: Every cardiac disease has a relation with one or many of them
Time : 14:05-14:50

Biography:
Sergio Mejía Viana has completed his Cardiology training and Doctorate at the University Clinic of Navarre. He was an interventional Cardiologist, Angiologist and Phlebologist for 20 years. He is a Fellow of the European Society of Cardiology, has written more than 100 scientific publications including abstracts, articles and book chapters. He returned to clinical practice with high interest in prevention. Currently, he is a Consultant at the Medical Investigation Unit in St. Bernard´s Hospital in Gibraltar.
Abstract:
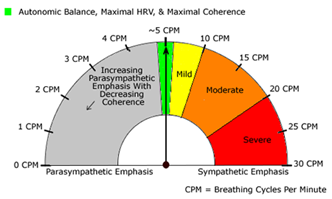
Stress is defined as a process in which environmental demands strain an organism’s adaptive capacity resulting in both psychological demands as well as biological changes that could place at risk for illness. Emotional stress is a major contributing factor to the six leading causes of death in the United States: cancer, coronary heart disease, accidental injuries, respiratory disorders, cirrhosis of the liver and suicide. According to statistics from Meridian Stress Management Consultancy in the U.K, almost 180,000 people in the U.K die each year from some form of stress-related illness. But our bodies are not only under emotional stress. Due to poor nutritional habits and environmental pollution we are constantly under the effect of a wide variety of chemical stressors which is defined as hazardous substances which, when released into an environment, damage the living organisms or ecosystems or reduces their ability to cope with environmental and biological changes (too many cups of coffee, too much alcohol, too much junk food, too many medications, inhaling substances at the factory or office, pollution on the road, smokers in your environment, etc.). We have also physical stress that is caused by, for example: pushing your body to the limits, working out at the gym, driving long distances continually, sitting in front of a computer for extended periods without breaks, gardening for long periods, any kind of labor intensive job, etc. There are additional definitions for mental, emotional and even spiritual stress. This workshop has the aim of providing the attendees with easy to learn tools to understand stress physiology, diagnosis and treatment using biologically effective methods like heart rate variability biofeedback that increase coherence between the parasympathetic and sympathetic nervous systems. Inputs on chemicals stressors like nutritional recommendations and knowledge on heavy metals will be discussed.
Recent Pubications:
- J. Pumpria, K. Howorka, D. Groves , M. Chester, J. Nolan, Functional Assessment of Heart Rate Variability: Physiological Basis and Practical Applications, International Journal of Cardiology 84 (2002).
- M. Biagini, C. Cammarota, M. Prisco, F. Di Liberato, V. Fiori, P. Greziosi, P. Perelli, R. Romano, M. Lanza, Autonomic Nervous System Function Assessed By Analysis of Heart Rate Variability At Rest and During Exercise In Hypertensive and Normotensive Subjects, American Journal of Hypertension, Volume 17, Issue 5, Supplement 1, May 2004..
- Heart Rate Variability Biofeedback, Self-Regulation, and Severe Brain Injury Sonya Kim, Ph.D., CRC, Joseph F. Rath, Ph.D., Rollin McCraty, Ph.D., Vance Zemon, Ph.D., Marie M. Cavallo, Ph.D., and Frederick W. Foley, Ph.D. Biofeedback Association for Applied Psychophysiology & Biofeedback Spring 2015, Volume 43, Issue 1, pp. 6–14..
- Azar B. Probing links between stress and cancer. APA Monitor Online. 1999;30:1–4..
- Greenberg JS. Comprehensive stress management. 7th ed. New York: McGraw-Hill; 2002.
- Klaudia Jomovaa, Marian Valkob. Advances in metal-induced oxidative stress and human disease. Toxicology 283 (2011) 65–87.
- Cardiac Nursing | Cardiac Surgery | Cardio-Oncology | Pediatric & Geriatric Cardiology | Interventional Cardiology | Hypertension
Location: Gatwick Hall

Chair
Antonis A Armoundas
Harvard Medical School, USA

Co-Chair
Athos Capuani
Private Organization Carrara, Italy
Session Introduction
Telmo Pereira
Polytechnic Institute of Coimbra, Portugal
Title: Early vascular aging (EVA) and lifestyle-based modulators (ADAM) of the vascular aging trajectory throughout life: Preliminary results of a community-based registry
Time : 14:45-15:10

Biography:
Telmo Pereira is a Senior Lecturer and Researcher at the Polytechnic Institute of Coimbra, Coimbra Health School, and is the Head of the Clinical Physiology Department. In the last five year, he has developed research in the areas of Cardiovascular Prevention and Neurosciences, and has also collaborated in the development of new non-invasive technology options for the assessment of vascular function.
Abstract:
In recent years, great emphasis has been placed on the role of arterial stiffness (AS) and central blood pressure (cBP) as measures of the cumulative effect of cardiovascular risk factors over the process of physiologic ageing. These parameters, currently labeled as arterial “tissue biomarkers”, were shown to be independent predictors for the development of cardiovascular (CV) diseases, and could thus increase the discriminative capacity when coupled to classic CV risk scores. Consequently, the assessment of AS and cBP are recommended as additional tests for the clinical evaluation of hypertensive patients (based on history, physical examination and findings from routine laboratory tests), for estimating the global cardiovascular risk in the overall population, and for describing the vascular ageing continuum.
Currently, the most widely employed methods for evaluating pulse waveforms are those based on applanation tonometry and transfer functions, although oscillometric blood pressure devices using specific algorithms for pulse wave analyses (PWA) have been proposed. At present, oscillometry is an affordable and reliable technique, and may allow a comfortable, accurate, repeated and prolonged estimation of arterial stiffness and central hemodynamics in daily life conditions, making it particular suitable for community-based follow-up intervention programmes, and for addressing the major questions underlined by the early vascular ageing (EVA) concept, namely: the validation of tissue biomarkers as surrogate end points for CV risk reduction; the determination of the predictive value of various of these arterial tissue biomarkers, and the discriminative improvement over conventional cardiovascular risk factors; the identification of effective and multidisciplinary actions to counteract the pathophysiological processes reflected in the EVA syndrome, particularly the aggressive decrease of atherosclerosis modifiers (ADAM). Hence, we designed a project to be implemented in a community setting based on the inter-play between Pharmacy Services, a Technology Company and a Research center, and the preliminary results will be presented.
Recent Publications:
- Picone DS, Schultz MG, Otahal P, Aakhus S, Al-Jumaily AM, Black JA, Bos WJ,Chambers JB, Chen CH, Cheng HM, Cremer A, Davies JE, Dwyer N, Gould BA, Hughes AD, Lacy PS, Laugesen E, Liang F, Melamed R, Muecke S, Ohte N, Okada S, Omboni S, Ott C, Peng X, Pereira T, Pucci G, Rajani R, Roberts-Thomson P, Rossen NB, Sueta D, Sinha MD, Schmieder RE, Smulyan H, Srikanth VK, Stewart R, Stouffer GA, Takazawa K, Wang J, Westerhof BE, Weber F, Weber T, Williams B, Yamada H, Yamamoto E, Sharman JE. Accuracy of Cuff-Measured Blood Pressure: Systematic Reviews and Meta-Analyses. J Am Coll Cardiol. 2017 Aug 1;70(5):572 586.
- Teixeira R, Monteiro R, Baptista R, Pereira T, Ribeiro MA, Gonçalves A, Cardim N, Gonçalves L. Aortic arch mechanics measured with two dimensional speckle tracking echocardiography. J Hypertens. 2017 Jul;35(7):1402-1410.
- Omboni S, Posokhov IN, Parati G, Avolio A, Rogoza AN, Kotovskaya YV, Mulè G, Muiesan ML, Orlova IA, Grigoricheva EA, Cardona Muñoz E, Zelveian PH, Pereira T, Peixoto Maldonado JM. Vascular Health Assessment of The Hypertensive Patients (VASOTENS) Registry: Study Protocol of an International, Web-Based Telemonitoring Registry for Ambulatory Blood Pressure and Arterial Stiffness. JMIR Res Protoc. 2016 Jun 29;5(2):e137. doi: 10.2196/resprot.5619.
- Pereira T, Pereira TS, Santos H, Correia C, Cardoso J. Arterial pulse pressure waveform monitoring by novel optical probe. Int J Cardiol. 2015 Jan 20;179:95-6.
- Pereira T, Santos I, Oliveira T, Vaz P, Pereira T, Santos H, Pereira H, Correia C, Cardoso J. Pulse pressure waveform estimation using distension profiling with contactless optical probe. Med Eng Phys. 2014 Nov;36(11):1515-20.
- Pereira T, Maldonado J, Coutinho R, Cardoso E, Laranjeiro M, Andrade I, Conde J. Invasive validation of the Complior Analyse in the assessment of central artery pressure curves: a methodological study. Blood Press Monit. 2014 Oct;19(5):280-7.
- Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, Boutouyrie P, Cameron J, Chen CH, Cruickshank JK, Hwang SJ, Lakatta EG, Laurent S, Maldonado J, Mitchell GF, Najjar SS, Newman AB, Ohishi M, Pannier B, Pereira T, Vasan RS, Shokawa T, Sutton-Tyrell K, Verbeke F, Wang KL, Webb DJ, Willum Hansen T, Zoungas S, McEniery CM, Cockcroft JR, Wilkinson IB. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014 Feb 25;63(7):636-46. doi: 10.1016/j.jacc.2013.09.063.
Bader Almustafa
Qatif Primary Health Care, Saudi Arabia
Title: Hypertension guidelines: Global review
Time : 15:10-15:35

Biography:
Bader Almustafa, MBBS, DPHC(RCGP), ABFM, SBFM, ECHS. After his graduate from medical school in 1989, he has done his postgraduate training in clinical pathology, family medicine, chronic care and hypertension in multiple institutions in KSA, UK, USA and Italy. Currently, he is a senior consultant Family physician and Clinical Hypertension Specialist in Qatif Primary Health Care, KSA. He has taking multiple leading responsibilities in multiple institutions. Currently, he is the General Secretary of the Saudi Hypertension Management Society, and the Middle East Representative of the World Hypertension League. Dr. Bader has developed and adapted multiple clinical and professional guidelines, and being engaged in multiple national and international scientific committees. Dr. Almustafa has carried out hundreds of training, quality improvement and research works in the management of hypertension and cardio-metabolic risk. He is having multiple published articles and books in the field of primary care and preventive cardiology, in particular. He has led and contributed in multiple international, regional and local work related to this field. He has been honored many times, for his work, regionally and internationally.
Abstract:
Since the mid-nineties, many professional bodies have issued their guidelines for the management of high blood pressure. In the current era, however, the modern telecommunication has made the dissemination of these guidelines easy and fast. It resulted, however, in creating confusion, where recommendations are conflicting or variable. This review presents the history of hypertension guidelines, worldwide, their agreements and variations, the queries addressed and those which are not.
The hypertension guidelines started as a disease-oriented targeting to control blood pressure, widened to have a more logic by approaching absolute cardiovascular risk, rather. Recently, multiple bodies have issued cardiovascular prevention guidelines combating multiple cardiovascular risk factors. This made the job of any practitioner difficult to follow which mandated a way to simplify the path from detection to control, in real practice. The cardiometabolic risk guideline is a novel approach to fill in this need.
In conclusion, though the disparities are many, all join the same concept. Disparities, however, may leave a lot of confusion among practitioners that need to be considered by guidelines developers. Translational guidelines, however, may abridge it.
Ram Sharony
Rabin Medical Center, Israel
Title: Treatment of mitral bio-prosthetic valve deterioration using trans-apical valve in valve technique: Intermediate-term outcomes
Time : 15:35-16:00

Biography:
Ram Sharony (born 1959), is the director of Minimally Invasive Cardiac Surgery at Rabin Medical Center, Israel. He is a graduate of Ben Gurion University. Ram finished the residency program in Cardiothoracic surgery (year 2000). As an attending surgeon he was recruited by Tel Aviv medical center and shortly thereafter he was sent to a fellowship at New York University (NYU), USA. In his first year he performed a basic research and focused on expression of Serin protease inhibitors and MAP kinases pathway in vein grafts remodeling and published his basic science research in leading scientific journals. In the second year of fellowship he focused on clinical activity of minimally invasive valve surgery. He published his clinical research on the topic of mitral valve repair, outcomes of AVR among patients with reduced LV function, and his manuscripts on the survival benefit of Off Pump CABG in patients with atheromatous aorta contribute to the popularity of this operation in this subset population. In addition, his papers regarding the advantages of minimally invasive AVR over median sternotomy has been cited by many authors and contributed to the development of less invasive approach. Since 2008, Dr. Sharony serves as the director of minimally invasive unit at Rabin Medical Center, Israel, where he performs various types of mitral valve operations (replacement or repair) and aortic valve surgeries via less invasive approach for patients from different places in Israel and international medical tourism. As part of his clinical activity he leads the collaboration with the invasive cardiologists (TAVI team) and performs surgical procedures with catheter valve technologies. In addition to transapical approach for TAVI, various type of mitral valve in valve operation has been performed at Rabin medical center including direct Sapien valve deployment in severe mitral annular calcification (MAC). He is the director of medical student’s program and the residency program. In addition to his contribution as chapter author in textbooks (including the chapter of acquired heart diseases in Schwartz's Principles of Surgery), Dr. Sharony has published on the topic of the myocardial protection (ischemic and pharmacologic preconditioning) and was involved in the research and development of heart assist device for the failing heart. His recent scientific activity is on the topics of valvular heart disease, mainly tricuspid valve and transcatheter valve procedures. Ram is a proctor of Perceval sutureless valve (Livanova, Italy) and have gained a large experience with rapid deployed valve in many international medical centers. He has been invited as a speaker and panel discussant in various scientific meetings.
Abstract:
Objective: The transcatheter approach for a failed bio-prosthetic valve is an emerging alternative to redo-valve surgery in patients at high surgical risk. We aim to analyze the mid-term outcomes of patients undergoing valve-in-valve implantation in the mitral position.
Methods: A dual center clinical experience in treating consecutive patients with symptomatic structural bio-prosthetic mitral valve deterioration using the valve-in-valve technique via the trans-apical approach. Outcomes were rigorously assessed and reported based on VARC 2 criteria definitions.
Results: The valve-in-valve procedure in the mitral position was performed in 30 patients, mean age 76±12 years, mean STS score 10.7±6.0. Balloon-expandable Sapien devices were used in all patients. The composite endpoint of device success was achieved in 29/29 (100%) of patients. The operative mortality was 3.5% (sepsis). Follow up (up to 6 years, mean 29 months) demonstrated survival rates of 90% and 83.3% during first and second year, respectively and remain constant afterward. Only one patient had cardiovascular related mortality (endocarditis) during this period. Most of surviving patients (96%) are in NYHA-FC I/II. No valve migration was observed. The mitral regurgitation degree among patients with predominant mitral regurgitation dropped immediately after the operation and remains constant during follow-up period (from 3.9±0.3 to 0.2±0.6 and 0.3±0.5, respectively. Post procedural mean mitral transvalvular gradient was 6.4±3.0 mmHg and remain constant during follow-up (6.3±1.6 mmHg, ns). Only one patient had mild para-valvular (PVL) leak. All other patients had no PVL. The pre-operative pulmonary artery pressure decreased from 67.2±18.4 to 43.8±11.2 at follow-up (p>0.01).
Conclusions: Intermediate-term clinical outcomes of transcatheter valve-in-valve implantation for the treatment of mitral prosthetic valve deterioration in high risk patient are encouraging. Despite significant clinical improvement, a residual elevated gradient across the valve, unrelated to the original deteriorated valve size were observed. This novel approach allows good survival rate and satisfactory quality of life during mid-term follow-up period.
Gulzhan Myrzakhmetova
National Research Center for Cardiac Surgery, Kazakhstan
Title: Rejection of the transplanted heart: What can we do to diagnosis?
Time : 16:15-16:40
Biography:
Gulzhan Myrzakhmetova is a cardiologist, candidate of Medical Science. She graduated from Almaty State Medical Institute in General Medicine. She has extensive work experience at regional cardiology hospitals. She has published more than 20 research articles. Her research interest includes heart transplantation, MSC and HF.
Abstract:
Introduction: The gold standard of diagnosis of rejection after HTX is endomyocardial biopsy. However, non-invasive methods for the early diagnosis of rejection reactions are currently being studied. With the improvement of the possibilities of ultrasound diagnosis of heart function, it becomes possible to study longitudinal deformation of the myocardium, as an early marker of violations of the contractile function of the heart.
Objective: To determine the possibilities of ultrasound TDI and strain heart rate as early markers of graft rejection.
Method: Patients n=32 after HTX were divided into two groups according to the results of EMB. The first group (1R, 2R) n=23 patients (20 men, the average age was 41±1.2 y); the second group (3R) n=9 patients (seven men, the average age 44±2.6 y). The duration of EMB after transplantation was 4-60 months. Survey methods: TDI and strain (Epic Q7 Philips). EMB signs of rejection of the humoral type (immunofluorescence study) and cellular (perivascular and interstitial infiltrate with or without necrosis and fibrosis).
Results: In case of TDI, there was no reliable difference between the two groups: mean Smed: 7.81±1.7 cm/s vs. 7.97±2.1 cm/s and mean Slat: 8.78±2.18 cm/s against 8.4±1.45 cm/s (as p=NS). However, the mean longitudinal strain of the left ventricle (strain) in the first group (-16.5±0.9) was significantly higher in comparison with the second group (-12.2±1.2), (p<0.05). Sensitivity and specificity for longitudinal deformation were 68% and 46%, respectively. In all patients (n=5, 1gp-1, 2g-4) with vasculopathy detected with CAG, the mean longitudinal deformation of the LV is decreased (strain-13.3).
Conclusion: Strain can be considered as a non-invasive marker of chronic transplant rejection and vasculopathy after cardiac transplantation.
Jacob Jamesraj
Madras Medical Mission, India
Title: Beating heart simulator: Conquest of cardiac motion
Time : 16:40-17:05

Biography:
Jacob Jamesraj is a senior cardiac surgeon with a special interest in teaching and teaching aids. He has designed training kits for training surgeons in coronary surgery including beating heart surgery, valve replacements and repairs and minimally invasive surgery. He conducts wet lab workshops and conferences. He is well published. He is an avid poet and painter.
Abstract:
Simulators have gained an important role in cardiac surgical training. Beating heart surgery is demanding in terms of technical skills. The role of simulators hence cannot be overemphasised. Simulating Cardiac motion credibly as to provide an apt practice atmosphere has been a challenge. Over the years we have designed many simulators and here we trace the steps that led to the most credible simulation of cardiac motion.
The initial simulators were motionless emphasizing only the varied positions. Tilting platforms came up next but were a poor design and the movements had no similarity to that of the heart. The next phase saw the inflatable balloon which was placed in the left ventricle and inflated and deflated using motorized bellows. This was the reverse of the actual cardiac motion and hence the design was changed. We used a motorized arm to move that of the stabilizer using a double ring linkage. This provided a more credible systole and diastole. Varying the positions and using a rheostat we could vary the heart rate and range of motion. This model offers more meaningful practice to the aspiring beating heart surgeon.
