Day 1 :
Keynote Forum
Gary L. Murray
Heart and Vascular Institute- Germantown & International College of Angiology, USA
Keynote: The potential role of a unique, simple, quick, accurate, inexpensive, routine evaluation of autonomic nervous system sympathetic (S) and parasympathetic (P) activity in cardiovascular diseases
Time : 08:35-09:10

Biography:
Gary L Murray received a Phi Beta Kappa Bachelor’s degree from Rhodes College, Memphis, USA. He received Belk Bible Award for the most outstanding Bible student. After graduating from Tulane University School of Medicine, New Orleans, USA, his Post-doctoral training was at University of Tennessee Center of Health Care Sciences, Memphis, USA. He became Co-director of Cardiac Catheterization as well as Nuclear Cardiology laboratories at Baptist Hospital, Memphis, USA. He then became Chief of Medicine, North Las Vegas, USA. Since, he has been in private practice in Memphis, yet he has managed to publish several articles and co-created the Shad-Murray first pass RNA exercise test for coronary disease that was employed at many centers in the USA and Europe. He participated in clinical trials of first elective coronary stent, as well as the first coronary atherectomy and laser devices. His ANS studies have been cited in the new textbook on clinical autonomic disorders by Colombo. He has spoken in several countries worldwide. He is currently Director of Research at Heart and Vascular Institute, Germantown, USA.
Abstract:
Evaluation of the important role of autonomic nervous system (ANS) plays in the development, progression, treatment and prognosis of cardiovascular diseases (CVD) has not been routine in clinical practice. However, new studies using a unique, easily applied technology have demonstrated the importance of ANS measures in the management of patients with risk factors for CVD, hypertension, orthostatic hypotension, congestive heart failure, and coronary disease. This new, unique technique and results of many studies will be discussed in detail. It is suggested that ANS measurement should be routinely used in CVD clinics, improving outcomes and lowering costs.
Keynote Forum
Antonio Bayés de Luna
Autonomous University of Barcelona & St. Pau Hospital, Spain
Keynote: Clinical implications of advanced interatrial block
Time : 09:10-09:45

Biography:
Antonio Bayés de Luna has been full Professor of Cardiology of Autonomous University of Barcelona, and Chairman of Cardiac Department of St. Pau Hospital of Barcelona. He has been President of Catalan, Spanish, and World Heart Federation, and also President of International Society of Cardiovascular Pharmacotherapy (ISCP). He has received many awards, including “Metge de l’any” from Catalonia, “Médico del año” of Spain (two times), “Creu de Sant Jordi” award of Generalitat of Catalonia, and “Premio Jaime I” of Generalitat of Valencia. He is member of more than 20 national societies of cardiology. He has published 306 papers, and just in the last 20 years, he has achieved H factor of 32. The number of references is more of 5.000. He has published more than 20 books, 10 as unique author. His book Clinical Electrocardiography has been translated to 10 languages.
Abstract:
The patients with advanced interatrial block (A-IAB) (P≥120ms plus±pattern in II, III and aVF) present more frequently atrial fibrillation (Bayes syndrome) and even stroke and dementia. The following considerations have to be considered: AF is not the final cause of stroke; atrial fibrotic CM is the substrate of both AF and A-IAB; there are many similarities between these two processes. Very often A-IAB is a precursor of AF and both may be considered mediators of stroke; there is a clear evidence that A-IAB and AF are risk factors of stroke, and even dementia, and global, CV, and sudden death; in a group of patients in SR (A-IAB) that are risk factors of AF and stroke, we have to perform a randomized to demonstrate the benefits to anti-coagulate patients in SN without documented AF; if this trial is positive, we have to establish a score of risk of stroke for patients in sinus rhythm to be used at a global level; until then, we can take decisions at individual level according to the careful observations of ECG (P-wave) and other
parameters (CHA2DS2-V, ambiental arrhythmias, detection of fibrosis, etc.).
Recent Publications
1. Bacharova L and Wagner G S (2015) The time for naming the inter-atrial block syndrome: Bayes Syndrome. J Electrocardiol
48:133-134.
2. Martínez-Sellés M, Massó-van Roessel A, Álvarez-Garcia J, Garcia de la Villa B, Cruz-Jentoft A, Vidán M T, López J, Felix-Redondo F J, Durán J M, Bayés-Genís A, Bayés de Luna A (2016) The investigators of the Cardiac and Clinical Characterization of Centenarians (4C) registry; inter-atrial block and atrial arrhythmias in centenarians: prevalence, associations, and clinical implications. Heart Rhythm 13:645-651.
3. Fabritz L (2016) The power of P in the elderly: small biphasic wave, big impact. Heart Rhythm 13(3):653.
4. Enriquez A, Sarrias A, Villuendas R, Ali F S, Conde D, Hopman W M, Redfearn D P, Michael K, Simpson C, De Luna A B, Bayes-Genis A and Baranchuk A (2015) New-onset atrial fibrillation after cavotricuspid isthmus ablation: identification of advanced inter-atrial block is key. Europace 17:1289-1293.
5. Bayés de Luna A, Martínez-Sellés M, Bayés-Genís A, Elosua R and Baranchuk A (2017) Surface ECG inter-atrial blockguided treatment for stroke prevention: rationale for an attractive hypothesis. BMC Cardiovascular Disorders 17:211.
Keynote Forum
Sergey Suchkov
Sechenov University, Russia
Keynote: Personalized and translational medicine as a model of the healthcare services and armamentarium to get the model armed: Myth or the reality?
Time : 09:45-10:20

Biography:
Sergey Suchkov completed his Graduation from Astrakhan State Medical University; MD and PhD. He worked for Helmholtz Eye Research Institute and Moscow Regional Clinical Research Institute (MONIKI). He was a Secretary-in-Chief of the editorial board, Biomedical Science, an international journal published jointly by the USSR Academy of Sciences and the Royal Society of Chemistry, UK. At present, he is Director at Center for Personalized Medi-cine, Sechenov University; Chair in the Department for Translational Medicine, Moscow En-gineering Physical University (MAPhI) and; Secretary General at United Cultural Convention (UCC), Cambridge, UK. He is a member of the New York Academy of Sciences, American Chemical Society (ACS), American Heart Association (AHA), AMEE, Dundee, UK, EPMA, Brussels, EU, PMC, Washington, DC, USA and ISPM, Tokyo, Japan.
Abstract:
A new systems approach to diseased states and wellness result in a new branch in the healthcare services, namely, personalized medicine (PM). To achieve the implementation of PM concept into the daily practice including clinical cardiology, it is necessary to create a fundamentally new strategy based upon the subclinical recognition of bio-indicators (bio-predictors and biomarkers) of hidden abnormalities long before the disease clinically mani-fests itself. Each decision-maker values the impact of their decision to use PM on their own budget and well-being, which may not necessarily be optimal for society as a whole. It would be extremely useful to integrate data harvesting from different databanks for applications such as prediction and personalization of further treatment to thus provide more tailored measures for the patients and persons-at-risk resulting in improved outcomes whilst securing the healthy state and wellness, reduced adverse events, and more cost effective use of health care resources. One of the most advanced areas in cardiology is atherosclerosis, cardiovascular and coronary disorders as well as in myocarditis. A lack of medical guidelines has been identified by the majority of responders as the predominant barrier for adoption, indicating a need for the development of best practices and guidelines to support the implementation of PM into the daily practice of cardiologists! Implementation of PM requires a lot before the current model “physician-patient” could be gradually displaced by a new model “medical ad-visor-healthy person-at-risk”. This is the reason for developing global scientific, clinical, social, and educational projects in the area of PM to elicit the content of new branch.
Recent Publications
1. T A Bodrova, D S Kostyushev, E N Antonova, Sh Slavin, D A Gnatenko, M O Bo-charova, M Legg, P Pozzilli and S V Suchkov (2012) Introduction into PPPM as a new paradigm of public health service: an integrative view. EPMA Journal 3(16):3-16.
2. I A Sadkovsky, O Golubnitschaja, M A Mandrik, M A Studne-va, H Abe, H Schroeder, E N Antono-va, F Betsou, T A Bodrova, K Payne and S V Suchkov (2014) Predictive, Preventive and Personalized Medicine (PPPM) as a new model of the National and International Healthcare Services and thus a promising strategy to prevent a disease: from basics to practice. International Journal of Clinical Medicine 5:855-870.
3. Zemskov V M, Alekseev A A, Gnatenko D A, Kozlova M N, Shishkina N S, Zemskov A M, Zhegalova I V, Bleykhman D A, Bahov N I and Suchkov S V (2016) Overexpression of Nitric oxide synthase re-stores circulating angiogenic cell function in patients with coronary artery disease: implications for autologous cell therapy for myocardial infarction. The Journal of the American Heart Association 5:1-18.
4. Zemskov A, Zemskov V, Zemskova V, Buch T, Cherno-va L, Bleykhman D, Marshall T, Abe H, Zhegalova I, Barach P and Suchkov S (2017) A stepwise screening protocol to secure the module-based treatment for managing immunopathology. International Journal of Information Research and Review 4(1):3507-3510.
Keynote Forum
Nobuhiro Handa
Pharmaceuticals and Medical Devices Agency, Japan
Keynote: Nationwide registries associated with cardiovascular medical devices in Japan
Time : 10:20-10:55

Biography:
Nobuhiro Handa, M.D. is presently the Principal Reviewer, Office of Medical device, Pharmaceuticals and Medical Device Agency, Japan. He completed his education from Nada, Junior and Senior High School in1979, then joined The University of Tokyo, College of Art and Science up to 1981. After that he completed his medical doctor degree from The University of Tokyo, Faculty of Medicine in March 1985. He did his hospital training from various institutes. He received Special Certificate as a certified physician for using Zenith AAA Endoprosthesis in Japan. He has society membership to The Japanese Surgical Society, The Japanese Association for Thoracic Surgery, The Japanese Society of Artificial Organs, The Japanese Society of Ultrasound in Medicine and The Japanese society for Heart and Lung Transplant.
Abstract:
The accumulation of real world data associated with medical devices, or a medical device registry plays an important role in promoting the development of medical devices. It is desirable to utilize registry data for pre-approval review as well as postmarketing
safety measures. However, data has often been collected without compliance with a good clinical practice. Furthermore, the registry may not include all data elements required for demonstrating the effectiveness and safety of medical devices. As such, it may not meet the regulatory requirements for pre-market review. Despite these limitations, there are many national registries, such as orthopedic total hip joint registries in multiple countries that have successfully detected the increased revision rate of metal on metal hip implant. In addition, there are several national registries in the European Union, US and Japan that include registries for artificial heart placement, trans-catheter aortic valve replacement and devices for peripheral arterial diseases. If registry is nationwide, it is an unbiased real world data for the country. The outputs of the analyses can be compared with registries in other countries if the findings are consistent between countries or not. The current issues of registry management include ensuring a wide patient coverage, involvement of regulatory authority, implementing rules of data utilization by the manufacturer, regulators and the academic sector, and obtaining sustainable funding for registry management. In the presentation, we focus on the eight existing nationwide registries associated with cardiovascular medical devices in Japan and discuss their characteristics including data quality, data utilization and financial sustainability. Some of them were utilized for regulatory purposes. Early participation of regulators for developing a national registry and a system that assures accuracy of data seems to be a key element for their regulatory applications based on Japanese PMD-ACT. The cooperation between the academic sector, industry and regulatory bodies is essential for utilizing registry data efficiently.
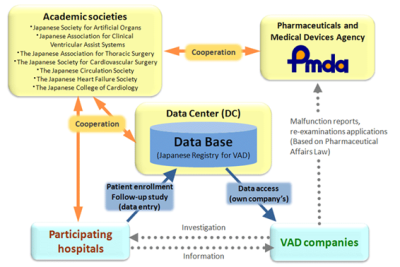
Figure 1: Registry framework of Japan mechanically assisted circulatory support
- Clinical Cardiology | Heart Diseases | Electrocardiography | Nuclear Cardiology | Diabetes & Heart | Women & Heart Disease
Location: Gatwick Hall

Chair
Gary L Murray
Heart and Vascular Institute, Germantown & International College of Angiology, USA

Co-Chair
Sergey Suchkov
Sechenov University, Russia
Session Introduction
Luis Martinez Millan
Achucarro Center for Neuroscience, Spain
Title: Geomagnetic fields produce trophic effects in myocardium
Time : 11:10-11:35

Biography:
Luis Martinez Millan is PhD in Medicine and specialized in Pediatrics. Since 1992 is Full Professor in Human Anatomy and Embryology. His research is centered on development and plasticity of sensory systems, documenting the reorganization of sensory afferents after removal of visual inputs in young animals and enhancing the plastic possibilities after lesions in adult systems. In the last years he observed changes of gene expression in encephalic neurons under the influence of modified geomagnetic fields. And very recently he detected changes in blood vessels density and distribution in experimental animals submitted to modified geomagnetic fields. Presently he is Professor Emeritus adscribed to the Achucarro Center of Neurosciences in Lejona (Spain).
Abstract:
Changes of 100 degrees in the orientation of the horizontal vector of a geomagnetic field produced by three pairs of Helmholtz coils cause unanticipated alterations in the brain as well as the heart. In the rodent brain, it leads to significant cfos expression in cortical and subcortical brain structures. This expression requires neurotransmitter secretion and is mediated by the MAPKinases pathway. In the heart, autonomous and cholinergic cardiac innervations are responsible for a permanent electrical activity that makes the myocardium a receptor for magnetic fields actions. Mice submitted to the same aforementioned modified geomagnetic fields for one hour every 8 hours during a period of 10 days caused a cardiac hypertrophy. This was mainly due to a considerable increase of myocardic blood vessels distributed in both ventricles, as well as, in the intermediate and deep myocardic strata. Moreover, significant increase of cfos expression was detected in treated cases in comparison with controls. Vasculoepithelial growth factor participates in the higher density of vessels. Although these preliminary results have to be completed by studying time course, persistency and appearance after experimental myocardial infarction, it suggests the potential towards alternative clinical therapies and a translational value. The added benefit is that the magnetic apparatus is inexpensive and the envisaged application to human patients would be non-invasive.
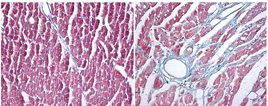
Left pricture shows the left ventricle of a control animal and the right one shows the left ventricle of a treated animal
Recent Publications:
- Actions of weak magnetic fields on signaling molecules in biological systems. JL Zugaza, JM Barandiaran, F Zallo, D Sanchez and L Martinez Millan. 5th European Conference on Molecular Magnetism (ECMM) 6-10 September Zaragoza Spain 2015.
- MicroRNAs and nervous plasticity. L Martinez Millan. VI international Congress of Hstology and Tissue Engineering. 16-18 September Bilbao Spain 2015.
- Mechanisms involved in the gene expression changes induced by modified geomagnetic fields in encephalic neurons. L Martinez Millan, F Zallo, B Pinar, I Gerrikagoitia and JL Zugaza. 14th Meeting of the Society for Applied Neuroscience. Utrecht The Nederlands. 30th Jan-2nd Feb 2014.
- García Del Caño G; Gerrikagoitia I; Alonso-Cabria A; Martínez-Millán L.Organization and origin of the connection from the inferior to the superior colliculi in the rat.J Comp Neurol. 499 - 5, pp. 716 - 731. 2006.
- Gerrikagoitia I; Martínez-Millán L. Guanosine-Induced Synaptogenesis in the Adult Brain In Vivo. Issue The Anatomical Record.292-12,pp.1968-1975.2009.
Biji Soman
Sree Gokulam Medical College and Research Foundation, India
Title: Coronary angiographic profile of diabetic women with acute coronary syndrome in south India
Time : 11:35-12:00

Biography:
Major. Dr. Biji Soman graduated from Government Medical College, Trivandrum in 1996 served in the Indian Army as a Short Service Commission (SSC) officer for 5 years. Then he joined Sree Utharadom Thirunal (SUT) Hospital in Trivandrum, a reputed tertiary care cardiac centre as Registrar in Cardiology and Cardiac Catheterisation Lab. He went to United Kingdom in 2005 and trained at the prestigious Guy’s & St. Thomas’ NHS Trust Hospital, London in Cardiology. He did Post Graduate Diploma in Clinical Cardiology from Kerala Institute of Medical Sciences (KIMS), Trivandrum, passed out with Distinction and First Rank in Kerala state. He obtained Membership of Royal College of Physicians (MRCP UK) in 2013. He became substantive Consultant Cardiologist in 2014; was elected as a collegiate member of Royal College of Physicians and Surgeons of Glasgow MRCPS (Glas) in 2014. He is presently affiliated with Sree Gokulam Medical College and Research Foundation Trivandrum as Consultant Cardiologist. He won awards for best paper presentations in National Conferences. He is the faculty in International and National conferences in Clinical Cardiology. He has several academic publications to his credit in both National and International peer reviewed Scientific Journals. His area of interest is cardiovascular diseases among women.
Abstract:
Objective: Diabetes mellitus is known to be a major risk factor for the development of coronary artery disease (CAD). The aim of this study was to assess and compare the extent and the severity of coronary artery disease (CAD) in diabetic and non diabetic women with acute coronary syndrome.
Methods: Angiographic findings of diabetic and non diabetic women, who presented with acute coronary syndrome were analysed and compared. Two interventional cardiologists, determined the presence and characteristics of atherosclerotic lesion, according to the American Heart Association classification.
Results: 283 women who presented with acute coronary syndrome were studied, of these 166 with mean age of 60.84 ± 9.49 years were diabetic and 117 with mean age of 58.70 ± 11.78 years were non diabetic. Unstable angina was significant among non diabetic women [99 vs. 84, p = 0.035, OR 1, (CI 0.349 – 0.965)], while ST elevation myocardial infarction (STEMI) was significantly higher among diabetic women [36 vs. 12, p = 0.012, OR 2.423 (CI 1.201 – 4.89)]. Diabetic women had higher incidence of triple vessel disease (TVD) [44 vs. 12, p < 0.001 OR 3.156, (CI 1.584 – 6.289)], while non diabetic women had higher incidence of angiographically normal epicardial coronary arteries [14 vs. 30, p <0.001 OR = 1, (CI 0.134 – 0.531)], segmental distribution showed proximal segment disease was the commonest, however, diabetic women had greater number of lesion per patient (2.47 vs. 1.31). Diabetics also had greater no. of left mainstem disease, though not statistically significant (10 vs. 3, p = 0.735). LAD was more commonly involved among non diabetic women (112 vs. 60, p = 0.007). Diabetics had greater type B2 [124 vs. 16, p < 0.001, OR = 3.692, (CI 2.113 – 6.449)] and type C [228 vs. 69, p = 0.027, OR = 1.514, (CI 1.047 – 2.190)] lesions, while non DM had greater percentage of type A [20 vs. 28, p < 0.001, OR= 1, (CI 0.126 – 0.423)] and B1 [48 vs. 44, p < 0.001, OR = 1 (CI 0.209 – 0.525)] lesions.
Conclusion: These findings confirm that the diabetic women have more severe and extensive coronary artery disease than the non diabetics, especially among south Indian women.
AM Thirugnanam
Virinchi Hospitals, India
Title: Comparison of new generation Everolimus eluting stents and new generation of Sirolimus eluting stents in chronic renal failure patients with 3 years outcome
Time : 12:00-12:25

Biography:
Dr. AM Thirugnanam, MD., MSICP, Ph (USA).FSCAI. (USA) is currently the senior interventional cardiologist at Virinchi Hospitals in Hyderabad, India. He did under-graduation in 1996 from Ashwood Medical University (Texas); Masters(MD) in internal medicine in 1999 from Belford University (Texas) and PhD (1999-2002) in interventional cardiology Ashwood Medical University. He has presented more than 150 research papers in national and international conferences, especially in cellular and interventional level. He had held various positions in national and international conferences. He had conducted many national conferences in Cardiology. He has been teaching non-invasive and Invasive cardiology to undergraduate and postgraduate medical students for the past six years and writing articles in indexed journals and media. He has been conducting monthly CME for doctors regularly on advanced cardiology topics with clinical experience which have been helping them in their day to day practice. He conducted research on advanced interventional pharmacology like Bivalirudin, prasugrel, GP2b3a RB in PCI.
Abstract:
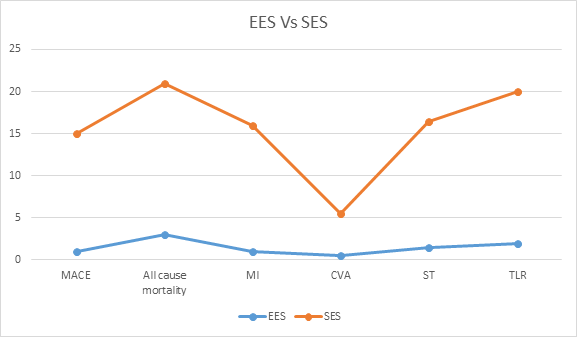
Background: This is follow up results of Use of new generation Everolimus and Sirolimus stents in chronic renal patients have been shown to reduce myocardial infarction, target vessel revascularization (TVR) and major adverse cardiovascular events (MACE), without increasing in bleeding risk in CKD patients.
Objective: Our aim to compare the safety and efficacy outcome between new generation Everolimus stent and Sirolimus eluting stents in patients undergoing PCI with New EES and SES.
Methods: We retrospectively analyzed 150 patients who underwent PCI in our centers, between August 2014 and August 2017. Patients were divided in to two groups: new EES (n=105) and new SES (n=45). Primary end points were at 1-year, 2-year, 3-year, composite of all cause of death, MI, CVA, TVR, MACE and stent thrombosis were also evaluated.
Results: Femoral access in 30% and 70% radial access were used. Rate of dual antiplatelet used 1 year were 96% in EES and 90% in SES. The primary end points occurred in 7% of EES and in 25% of SES. There were significant differences found with respect to the rate of 3 years all-cause mortality (3% vs 18%), MI (1% vs 15%), CVA (0.5% vs 5%), ST (1.5% vs 15%), TVR ( 2% vs 18%), MACE (1% vs 14%) and 2 cases of major bleeding were observed in SES patients and not in EES.
Conclusion: New EES stents shown very positive and encouraging results in CKD patients than new SES stents. This 3 years study may further be extended to evaluate very late events.
Višnja Nesek Adam
Clinical Hospital Sveti Duh & Josip Juraj Strossmayer University of Osijek, Croatia
Title: Propofol versus midazolam/fentanyl for elective electrical cardioversion
Time : 12:25-12:50

Biography:
Višnja Nesek Adam is anesthesiologist, emergency medicine specialist and subspecialist in intensive care medicine. She is recognised for her expertise in emergency medicine. Dr. Nesek served as Assistant Professor at JJ Strossmayer School of Medicine at the University of Osijek. Although she loves the clinical practice of anesthesia and emergency medicine, teaching students is her true passion and she was responsible for teaching medical students, residents and fellows about the anesthesia and emergency medicine. She is also Head of the University Department of anesthesiology, reanimatology and intensive care medicine and Center for emergency medicine.
Abstract:
Statement of the Problem: Elective cardioversion (EC) is a short procedure aim to return the heart to a normal rhythm following cardiac dysrhythmias. This procedure is extremely stimulating and painful and can be distressing for the patient; therefore anesthetists are often requested to provide anesthesia. The level of sedation required for cardioversion is either deep sedation or general anesthesia. Selection of the anesthetic agent is important, because a short duration of action, early recovery without complications and hemodynamic stability are required. This is particularly important in hemodynamically unstable patients. The purpose of this study was to compare propofol and midazolam – fentanyl combination for procedural sedation during EC.
Methodology & Theoretical Orientation: Patients older than 18 years, American Society of Anesthesiologists I-III grades undergoing elective cardioversion were randomly divided into one of two groups. Group P (n = 30) were received propofol 1 mg/kg intravenous (IV) bolus followed by 0.5 mg/kg. Group MF ( n = 30) were initially administered fentanyl (1.25 μg/kg IV), followed by a bolus of midazolam 3 mg IV and titrated to the sedation. Time to sedation and level of consciousness was assessed by subjective clinical signs of patients: incoherent speech, vertical nystagmus, glassy eyes, yawning and then muscular relaxation. During the procedures a change in heart rate, blood pressure, and respiratory pattern were also observed. We have recorded the time intervals needed for eyes opening (awakening time) and replay psycho-cognitive functions assessed by the patient’s ability to open his/her eyes upon command and to correctly pronounce the name.
Findings: Mean time to sedation was faster with propofol and patients in the propofol group had shorter mean times to wakening and full consciousness, but propofol was associated with a higher incidence of apnea.
Conclusion & Significance: The propofol provided satisfactory hemodynamic stability, along with shorter sedation and wakening. However, the advantage of shorter sedation and wakening times associated with propofol should be weighed against the possibility of adverse events, particularly respiratory depression.
Recent Publications:
- Gerstein NS, Young A, Schulman PM, Stecker EC, Jessel PM (2016) Sedation in the Electrophysiology Laboratory: A Multidisciplinary Review. J Am Heart Assoc. 13;5(6). pii: e003629. doi: 10.1161/JAHA.116.003629.
- Desai PM, Kane D, Sarkar MS (2015) Cardioversion: What to choose? Etomidate or propofol. Ann Card Anaesth 18:306-11. 2.
- Chung MY, Chea JS, Kim CJ, Lee BH (2001) Effect of Midazolam, Fentanyl and Propofol for Intravenous Anesthesia in Patients Undergoing the Cardioversion. Korean J Anesthesiol 41(3):284.
- Tang RB, Dong JZ, Zhao WD, Liu XP, Kang JP, Long DY, Yu RH, Hu FL, Liu XH, Ma CS (2007).
- Unconscious sedation/analgesia with propofol versus conscious sedation with fentanyl/midazolam for catheter ablation of atrial fibrillation: a prospective, randomized study. Chin Med J 120:2036–2038. Zed PJ, Abu-Laban RB, Chan WW, Harrison DW (2007) Efficacy, safety and patient satisfaction of propofol for procedural sedation and analgesia in the emergency department: a prospective study. CJEM. 9(6):421-7.
- Special Session
Location: Gatwick Hall
Session Introduction
Fabiola B Sozzi
Staff Cardiologist, Ospedale Maggiore Policlinico CÃ Granda, Italy
Title: Diastology: Pathophysiology of relaxation and filling pressure
Time : 14:00-14:45

Biography:
Dr. Fabiola Sozzi works as a staff cardiologist at the University Hospital Policlinico of Milan, Italy, with high-specialization nomination. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She gained a high expertise in echocardiography at the Thoraxcentre of Rotterdam (NL), where she defended the PhD thesis on stress cardiac imaging under the supervision of Professor J. Roelandt. She is Visiting Professor at the University of Milan where she leads several research projects and teaches at the Faculty of Medicine and School of Specialization of Cardiology. She is author of 70 papers published in indexed peer-reviewed international journals and reviewer of several medical international journals.
Abstract:
Doppler echocardiography can characterize left ventricular diastolic function through a combination of measurements, which show evidence of slowed ventricular relaxation, increased left ventricular stiffness or abnormal left ventricular filling. Doppler echocardiography can also provide an estimate of left ventricular filling pressures, one component of diastolic function that reflects pulmonary capillary wedge pressure. These parameters have been shown to correlate with exercise capacity.
A normal diastolic function response to exercise is characterized by normal and similar resting and exercise E/e’ measurements. Elevated left ventricular filling pressure is a cardinal feature of heart failure with preserved ejection fraction (HFpEF). The ratio of transmitral E to mitral annular e′ velocities (E/e′) at Doppler echocardiography has been proposed as a non-invasive measure of left ventricular filling pressure and endorsed by professional guidelines as a surrogate parameter of invasive left ventricular filling pressure in the diagnostic work-up of HFpEF. The diagnosis of HFpEF is straightforward when patients are acutely decompensated. To make matters more complex, many patients with HFpEF display normal left ventricular filling pressures at rest, with abnormalities that develop during stresses like exercise.
Invasive hemodynamic exercise testing has emerged as the gold standard to diagnose or exclude HFpEF in patients with exertional dyspnea of unclear etiology, but cost, risk, and the requirement for specialized training and equipment may limit its broad application in practice and in clinical trials. Therefore, Doppler echocardiography plays a central role in the non-invasive evaluation and grading of diastolic dysfunction.
The American College of Cardiology Foundation/American Heart Association guidelines define HFpEF as clinical signs and symptoms of HF, preserved ejection fraction, and no other obvious explanation for symptoms. This scheme works well for patients with a high likelihood of disease on the basis of clinical indicators of congestion. To address the patients without overt congestion, more recent guideline statements from the European Society of Cardiology (ESC) and American Society of Echocardiography/European Association of Cardiovascular Imaging (ASE/EACVI) require objective evidence of high left ventricular filling pressures.
Recent Publications:
- Hiroyuki O, Hiiroo I, Miyo T, et al. Impact of Doppler derived left ventricular diastolicperformance on exercise capacity in normal individuals. Am Heart J 2000;139(4):716–722.
- Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32:670-679.
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200.
- Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009; 10:165-193.
- Heart Diseases | Clinical Cardiology | Electrocardiography | Nuclear Cardiology | Diabetes & Heart | Women & Heart Disease
Location: Gatwick Hall

Chair
Gary L Murray
Heart and Vascular Institute, Germantown & International College of Angiology, USA

Co-Chair
Sergey Suchkov
Sechenov University, Russia
Session Introduction
Jochen Senges
Stiftung Institut für Herzinfarktforschung Ludwigshafen, Germany
Title: Mass media campaign to improve poor diagnosis and poor medical adherence in atrial fibrillation
Time : 14:35-15:00

Biography:
Jochen Senges is the Director of the Institute of Herzinfarktforschung Ludwigshafen. He completed his Medical School at University of Heidelberg, Berlin and Frankfurt 1961-1966; Medical Diploma at University of Heidelberg in 1966; Board certification in Internal Medicine in 1974. He was a Senior Staff Physician in Department of Cardiology, University of Heidelberg. He completed his PhD in Medicine with a neurophysiologic dissertation at University of Heidelberg in 1967 and; was a Research Fellow at Stanford University, California, USA in 1969. His main research topic is Cardiac Arrhythmias. He was an Associate Professor of the Medical Faculty, University of Heidelberg in 1981.
Abstract:
Atrial fibrillation (AF) is the most common cardiac rhythm disorder and affects mainly older people. Poor diagnosis of AF: Large registries (Gloria-AF) have clearly shown that about two-third of patients in Western Europe with newly diagnostic non valvular AF are detected asymptomatic/minimally symptomatic. The rate of previous stroke in these patients is more than twice as high as in symptomatic patients, despite no difference in CHA2DS2-VASc-Score. This may be explained by a longer but subclinical and therefore undiagnosed AF history. Poor medical adherence: poor medication adherence is the second most important factor underlying strokes in patients with atrial fibrillation. Various major studies have demonstrated that less than half of AF-patients are treated with guideline antithrombotic medication. Mass media campaign: these results underline the importance for both: public programs to detect non-valvular AF in the older population but also public education programs that should focus on patients’ poor understanding of the importance for sustained antithrombotic medication adherence to prevent stroke. The ARENA study includes a longstanding mass media campaign over one year to improve diagnosis and medical adherence in atrial fibrillation. Actually over 10.000 AF-patients are documented and first results will be presented at this meeting.
Recent Publications
1. Puls Miriam, Lubos Edith, Boekstegers Peter, Bardeleben Ralph Stephan von, Ouarrak Taoufik, Butter Christian, et al., (2016) One-year outcomes and predictors of mortality after MitraClip therapy in contemporary clinical practice: results from the German transcatheter mitral valve interventions registry. Eur Heart J 37(8):703–712.
2. Schmidt Martin, Dorwarth Uwe, Andresen Dietrich, Brachmann Johannes, et al., (2016) German ablation registry: cryoballoon vs. radiofrequency ablation in paroxysmal atrial fibrillation-one-year outcome data. Heart Rhythm 13(4):836–844.
3. Zylla Maura M, Brachmann Johannes, Lewalter Thorsten, Hoffmann Ellen, Kuck Karl-Heinz et al., (2016) Sex-related outcome of atrial fibrillation ablation - insights from the German ablation registry. Heart Rhythm 13(9):1837–1844.
4. Brachmann Johannes, Lewalter Thorsten, Kuck Karl-Heinz, et al., (2017) Long-term symptom improvement and patient satisfaction following catheter ablation of supraventricular tachycardia: insights from the German ablation registry. Eur Heart J 38(17):1317–1326.
Arash Gharehbaghi
Mälardalen University, Sweden
Title: Potentials of the intelligent phonocardiography as an emerging approach in cardiac assessments
Time : 15:00-15:25

Biography:
Arash Gharehbaghi received the M.S of biomedical engineering, on screening valvular and septal defects using heart sound signal analysis, from Amir Kabir University, Tehran, Iran, in 2000. He had been the head of the two research projects on cardiac signal analysis, between 2004 to 2008, that led to the international and domestic patents. He received his second M.S, on detecting ejection click from heart sound signal, from the Mon University, Belgium, in 2010, and his PhD degree from the Linköping University, Sweden, on severity assessment of valvular aortic stenosis using phonocardiography, in 2014. He is currently a research leader at Mälardalen University with the rise of coronary artery detection using intelligent phonocardiography.
Abstract:
Recent progresses in artificial intelligence made development of efficient decision support systems feasible. Application of such the DSS is rather seen in primary healthcare centers where accuracy of cardiac diagnosis is substantially low because of the complexities of cardiac auscultation. Our longstanding studies on heart sound analysis resulted in the novel methods that can provide sufficient means to extract significant medical information from the sounds to help the physicians in decision making. These methods were incorporated into a stand-alone system composed of an electronic stethoscope in conjunction with a portable computer. The resulted system, which we called the Intelligent phonocardiography (IPCG), provides an easy-to-use and inexpensive approach for cardiac assessments. Both the accuracy and the sensitivity of the IPCG in screening children with congenital heart disease were estimated to be higher than 87.0%, when a patient population of more than 250 individuals was employed. In a separate study, performance of the IPCG was investigated for assessing severity of valvular aortic stenosis in elderly patients, and the reliability and accuracy of the approach were estimated to be more than 80%. It is worth noting that screening patients with aortic stenosis based on IPCG had already been studied, where an accuracy of higher than 85% was achieved. Potential of the IPCG for pediatric cardiac assessments was rather studied in disease identification and also in discrimination between different cardiac defects with the systolic murmurs. Screening of the children with isolated bicuspid aortic valve, ventricular septal defect, and discrimination between valuvar aortic and pulmonic stenosis are considered as the examples of such studies. Results show that the IPCG has a high potential to be used in primary healthcare centers as an efficient decision support system. This can drastically reduce unnecessary echocardiography which is by far a more expensive approach.
Recent Publications:
- Gharehbaghi A, et al (2015) Assessment of aortic valve stenosis severity using intelligent phonocardiography. International Journal of Cardiology 198:58-60.
- Gharehbaghi A, et al (2017) A Deep Machine Learning Method for Classifying Cyclic Time Series of Biological Signals Using Time-Growing Neural Network, under press.
- Sepehri A, et al (2016) An intelligent phonocardiography for automated screening of pediatric heart diseases, Journal of Medical SYstems 40(1).
- Gharehbaghi A, et al (2017), Intelligent phonocardiography for screening ventricular septal defect using time growing neural network, Informatics Empowers Healthcare Transformation 238:108.
- Gharehbaghi A, et al (2015) An intelligent method for discrimination between aortic and pulmonary stenosis using phonocardiogram, World Congress on Medical Physics and Biomedical Engineering 1010-1013.
- Gharehbaghi A, et al (2015) A novel method for screening children with isolated bicuspid aortic valve, Cardiovascular Engineering and Technology, 6(4):546-556.
Maja Karaman Ilic
Clinical Hospital Sveti Duh & Josip Juraj Strossmayer University of Osijek, Croatia
Title: Lung ultrasonography for detecting fluid overload in intensive care patients early after surgery: A preliminary study
Time : 15:25-15:50

Biography:
Maja Karaman Ilić, PhD is an Anesthesiologist and IC Medicine Specialist presently working in Clinical Hospital Sveti Duh, Zagreb, Croatia. She is the assistant of Faculty of Medicine, JJ Strossmayer University of Osijek, Croatia. Her expertise has been focused on validation of non-invasive monitoring in volume status estimation of patients in Intensive Care Unit.
Abstract:
Aim: To investigate whether lung ultrasound can be used to detect fluid overload in the intensive care unit early after surgery.
Methods: This prospective study involved 60 patients without known cardiac or pulmonary diseases admitted to the intensive care unit at our Hospital after elective abdominal or vascular surgery. The inferior vena cava collapsibility index (IVCcl), PaO2/FiO2 ratio, and appearance of B-lines were determined upon admission to the intensive care unit and at 6, 12, and 24 h later. Fluid overload was de ned as IVCcl ≤ 40% and the presence of B-lines ≤7 mm. Tissue oxygenation impairment was defined as a PaO2/FiO2 ratio < 200.
Results: Fluid overload was detected in 42 patients (70%). The combination of dense B-lines and IVCcl ≤40% predicted fluid overload around the same time as drop of PaO2/FiO2 ratio (p = 0.115). Appearance of dense B lines correlated strongly with PaO2/FiO2 ratio (p < 0.001), while IVCcl did not correlate with PaO2/FiO2ratio (p = 0.071).
Conclusion: Our preliminary results suggest that lung ultrasonography may be a promising non-invasive method for early detection of fluid overload in spontaneous breathing intensive care patients soon after surgery. Our findings should be verified in larger studies.
Sergio Mejia Viana
St. Bernard´s Hospital, Gibraltar
Title: Heavy metals and atherosclerosis: One step forward in cardiovascular prevention
Time : 16:05-16:30

Biography:
Sergio Mejía Viana has completed his Cardiology training and Doctorate at the University Clinic of Navarre. He was an interventional Cardiologist, Angiologist and Phlebologist for 20 years. He is a Fellow of the European Society of Cardiology, has written more than 100 scientific publications including abstracts, articles and book chapters. He returned to clinical practice with high interest in prevention. Currently, he is a Consultant at the Medical Investigation Unit in St. Bernard´s Hospital in Gibraltar.
Abstract:
Atherosclerosis is not a single disease entity. In fact, the lesions of atherosclerosis represent a common response of the artery to numerous and potentially different forms of insult. Examination of atherosclerotic lesions reveal that each lesion contains the elements of an inflammatory response together with varying levels of fibro proliferative response. Many authors have written extensively about the holes in the cholesterol theory, and that mainstream medicine´s obsession with reducing cholesterol levels has always been misguided. There is increasing concern regarding the health effects of exposure to various heavy metals in the environment. This is particularly true for mercury, cadmium, lead, aluminum and arsenic. Lead exposure increased through the mid 1970´s, largely as a result of use of tetraethyl lead in gasoline. At the peak of lead production, the atmospheric release of lead reached 600.000 tons annually. The half-life of lead in the body is extremely long as it accumulates in the bone. The association between lead and cardiovascular disease has been recognized for years and there is consistent epidemiological evidence that lead is an established risk factor for hypertension, promotes oxidative stress and inflammation, the triggering event of atherosclerosis. Cadmium production increased during the 20th century as a result of the production of nickel-cadmium batteries, metal coatings and plastic stabilizers. Food and smoking are the major sources of cadmium for the general population. Cadmium is stored in the kidneys, liver, lungs, pancreas and central nervous system, with a half-life of over 15 years. A recent systematic review concluded that the evidence supports the role of cadmium as a cardiovascular disease risk factor, especially for coronary disease. Understanding that atherosclerosis is an inflammatory disease and not “fat deposits blocking arteries” will improve preventative strategies. The consequences of metal toxicity should now be published widely enough in order to avoid cardiovascular problems.
Recent Publications:
- Mejia Viana S (2015) From Framingham to Hunt 2: 60 Years Blaming the Wrong Culprit?. J Cardiol Curr Res 2015, 4(1): 00131.
- Nigra A,Ruiz-Hernandez A, Redon J, Navas-Acien A (2016) Environmental Metals and Cardiovascular Disease in Adults: A Systematic Review Beyond Lead and Cadmium. Current environmental health report December 2016, Volume 3, Issue 4, pp 416–433.
- Solenkova NV, Newman JD, Berger JS, Thurston G, Hochman JS, Lamas GA. Metal pollutants and cardiovascular disease: mechanisms and consequences of exposure. Am Heart J. 2014;168:812–22.
- Lamas GA, Navas-Acien A, Mark DB, Lee KL. Heavy metals, cardiovascular disease, and the unexpected benefits of edetate chelation therapy. J Am Coll Cardiol. 2016;67:2411–8.
- Huang Y-CT, Ghio AJ. Vascular effects of ambient pollutant particles and metals. Curr Vasc Pharmacol United Arab Emirates. 2006;4:199–203.
Sibel Catirli Enar
Memorial ÅžiÅŸli Hospital, Turkey
Title: Aortic valve diseases in pregnancy
Time : 16:30-16:55

Biography:
Sibel Catirli Enar completed her Graduation from Ä°stanbul University, Ä°stanbul Medical School in 1981. She has completed her specialization in Anesthesiology and Critical Care at Ä°stanbul Medical School in 1985 and in Cardiology at Ä°stanbul University Ä°nstitute of Cardiology in 1992. She became an Associate Professor of Cardiology in 2000, Fellow of European Society of Cardiology in 2010, Fellow of American Society of Echocardiography in 2012, Fellow of International Society of Cardiac Ultrasound in 2012 and Fellow of American College of Cardiology in 2016. She is working at Turkiye Hospital and Memorial Hospital in Istanbul, Turkey since 2000. She worked as a Research Fellow at Cleveland Clinic of Foundation, USA from 1996-1998 and at University of Alabama at Birmingham-USA from 2006-2008 as well. She has several publications in national and international journals. She served as speaker and moderator in national and international congresses. Her area of interest is Echocardiography.
Abstract:
Background: Stenotic rheumatic aortic valve diseases carry a higher risk in pregnancy. Regurgitant lesions are usually better tolerated. Mechanical valve prosthesis carry the risk of valve thrombosis and bleeding complications.Tissue valve prosthesis avoid the use of anticoagulants and thus, the complications.However,they are associated with higher risk of degeneration. According to ROPAC (The registry on pregnancy and cardiac disease), symptomatic and severe aortic stenosis carry a risk of heart failure and is associated with high rates of hospitalization for cardiac reasons. We report three cases: aortic mechanical valve, aortic homograft valve and severe aortic regurgitation in pregnancy.
Cases: Case 1 is a 30 years old female. She had undergone AVR due to rheumatic valvular disease.Valve thrombus occured in the first trimester and was successfuly resolved with tpa. Delivery was done with Ceaserean section (SC). There was some increase in her mitral regurgitation after the delivery. Baby had low birth weight,but no other complications occured.
Case 2 is a 25 years old female who had aortic homograft valve replacement for her bicuspid aortic valve. First pregnacy was uneventful.In her second pregnancy, aortic regurgitation was present and delivery was done with SC.She was treated medically. Case 3 is a 30 years old female who had rheumatic moderate aortic regurgitattion.During pregnancy, aortic regurgitation increased, and delivery was done with CS. After the delivery, aortic regurgitation decreased. No complications occurred with the baby.
Conclusion: Careful management of aortic valve diseases during pregnancy reduces complications. Even patients with mechanical prosthetic valves may be successfully treated. Mortality in pregnant women with aortic stenosis is very low. However,these patients carry a risk of heart failure which can be managed medically. Appropriate pre-conceptional patient evaluation and counseling is important in these patients.
Recent Publications:
- van Hagen IM, Roos-Hessenlink JW, Donvito V et al.(2017). Incidence and predictors of obstetric and fetal complications in women with structural heart disease. Heart 2017.
- Bons LR, Roos-Hesselink JW.(2016). Aortic disease and pregnancy. Curr Opin Cardiol.2016 Nov; 31(6):611-617.
- Orwat S, Diller GP, van Hagen IM et al.(2016).Risk of pregnancy in moderate and severe aortic stenosis: From the multinational ROPAC registry. J Am Coll Cardiol 2016 Oct 18; 68(16):1727-37.
- Sliwa K, Johnson MR, Zilla P, Roos-Hesselink JW.(2015).Management of valvular disease in pregnancy: A global perspective.(2015). Eur Heart J.2015 May 7; 36(18):1078-89.
- Carboni S, Capucci R, Pivato E et al.(2013). Marfan’s syndrome and pregnancy: A good maternal and fetal outcome. J Prenat Med.2013Apr; 7(2):21-4.
- De Santo LS, Romano G, della corte A et al.(2012).mechanical aortic valve replacement in young women planning on pregnancy: Maternal and fetal outcomes under low oral anticoagulation, a pilot observational study on a comprehensive pre-operative counselling protocol. J Am Coll Cardiol 2012 Mar 20; 59(12):1110-5.
Negar Omidi
Tehran Heart Center, Iran
Title: Does pregnancy mimic pathologic changes in electrocardiographic indices?
Time : 16:55-17:20

Biography:
Negar Omidi completed Masters (MD) in General medicine from Iran university of Medical Sciences, Tehran, Iran (1999-2007). She then specialized in cardiology from Shahid Beheshti University of Medical Sciences, Tehran, Iran (2009-2013). She worked in Tehran Heart Center and Ziaeian Hospital for quite a long time. She is currently the Assistant Professor in the Cardiology department of Tehran Heart Center, Tehran, Iran.
Abstract:
Introduction: Pregnancy can affect cardiac conduction system and make the pregnant women susceptible to arrhythmias, as increased susceptibility to atrial ones are common and ventricular arrhythmias are rare, but deadly.
Material and methods: Current study performed on 96 pregnant women, aged between 18 to 35 years, from 2015 to 2016. The sampling was simple convenient. Standard 12-lead surface electrocardiogram took at first trimester (2-nd month) and repeated on third trimester (8th month) and electrocardiographic indices calculated.
Results: The mean PR interval in T1 period was 133.36±20.9 ms and in T3 was 125.03±22.6ms (P =0.046).The mean QT in T1and T3 were 324.02±19.4ms 314.30±18.9ms respectively. (P <0.001).mean JT interval in T1 and T3 were 171.42±78.4ms and 166.48±75ms respectively (P=0.052). QRS duration in T1 and T3 were 98.02±9.1ms and 90.47±8.4 ms respectively (P=0.027). Mean of QTc (corrected QT interval) were 393.20±42.48 ms and 384.03± 23.2 in T1 and T3 respectively(P 0.023).
Discussion: According to our results mean parameters of electrocardiographic indices as PR, QT, RR, QRS and TP between two trimesters showed significant statistical differences. Mean of these indices reduced significantly, except JT and all of these indices were in normal range.
Recent Publications:
- Mehdizadeh M.Pasbakhsh P .Negar Omidi ; Nuropathological changes in the PDAPP transgenic mouse model of transgenic mouse of Alzheimers disease ; ACTA medica Iranica Journ; 2005; Vol 43, No 3.
- Pasbakhsh P. Negar Omidi. German DW ; Interaction of vesicular monoamine trasporter and neuromelanin pigment among the midbrain dopaminergic neurons in man; ACTA medica Iranica Journal ; 2009 ;47(4).
- Negar Omidi. Sharif Kashani M.Asad pour M . Khorghami MR.Ghorbani Y; The correlation of diastolic dysfuncion with TIMI frame count in patient s with chronic stable angina pectoris; Tehran University Medical Journal ; December 2012; Vol. 70; No. 9; 555-563.
- Tabib O.Khorghami, MR.Meraji . Negar Omidi .Mir Mesdagh. Accuracy of Doppler- derived indexes in prediction of pulmonary vascular resistance in children with pulmonary hypertension secondary to congenital heart disease with left to right shunt-Pediatric-Cardiology.Pediatric-Cardiology ; springer 2013;34.No. 7.
- Jamali Moghadam SR. Negar Omidi. Bayrami .Jamali Moghadam S. Ebola viral disease: a review literature; Asian Pacific Journal of Tropical Biomedicine ; April 2015; Volume 5, Issue 4 ; 260–267.

Biography:
Ali Al Bshabshe graduated from king Khalid university in Abha, Saudi Arabia in 2003, then he joined college of medicine and medical science, had Saudi board in internal medicine as well as Arab board and Jordanian board of internal medicine and the membership of the royal college of physician of the United Kingdom (MRCP UK). Fellowship training in adult critical care medicine at university of Ottawa Canada. Fellowship of the royal college of physician UK (FRCP). He is the associate professor of medicine at the department of medicine in college of medicine King Khalid University Abha, Saudi Arabia. adult critical care fellowship program director at southern region, Saudi Arabia. He was the former vice dean for clinical affairs, college of medicine King Khalid University Abha, Saudi Arabia.
Abstract:
Sepsis induced cardiomyopathy is an entity which most of the time overlooked by the practicing intensivist although it is not uncommon and good number critically ill septic patients might suffer from. There was a high incidence of severe sepsis attended in the ICU and high ICU and hospital mortality rates. Delayed diagnosis of sepsis and progression to multi organ failure which is associated with high mortality reported in the first 48 hours of ICU admission 1. Myocardial dysfunction is one of the main predictors of poor outcome in septic patients, with mortality rates next to 70%. 2. Severe sepsis and septic shock are the main cause of death in non-cardiac Intensive Care Units (ICU), with unacceptably high mortality rates 3. One of the proposed pathological mechanisms in sepsis induced cardiomyopathy is related to mitochondrial injury and dysfunction. 4. Oxidative stress leads to energetic (and thus functional) and structural failure of the cardiomyocyte. 5. Taken together, ROS derived from NOX1/NADPH oxidase play a pivotal role in endotoxin-induced cardiomyocyte apoptosis by increasing oxidation of Akt and subsequent de-phosphorylation by PP2A. Marked up-regulation of NOX1 may affect the risk of mortality under systemic inflammatory conditions. 6. In this proposed presentation, I will review the incidence of sepsis induced cardiomyopathy along with pathogenesis and recent literature related to the topic.
Recent Publications:
- Blanco J, Muriel-Bombín A, Sagredo V, et al. Incidence, organ dysfunction and mortality in severe sepsis: a Spanish multicentre study. Critical Care. 2008; 12(6): R158. doi:10.1186/cc7157.
- Romero-Bermejo FJ, Ruiz-Bailen M, Gil-Cebrian J, Huertos-Ranchal MJ. Sepsis-induced Cardiomyopathy. Current Cardiology Reviews. 2011;7(3):163-183. doi:10.2174/157340311798220494.
- Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005; 365:63–78.
- Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003; 348:1546–54.
- Tsolaki V, Makris D, Mantzarlis K, Zakynthinos E. Sepsis-Induced Cardiomyopathy: Oxidative Implications in the Initiation and Resolution of the Damage. Oxidative Medicine and Cellular Longevity. 2017; 2017:7393525. doi:10.1155/2017/7393525.
- Matsuno K., Iwata K., Matsumoto M., et al. NOX1/NADPH oxidase is involved in endotoxin-induced cardiomyocyte apoptosis. Free Radical Biology & Medicine. 2012;53(9):1718–1728. doi: 10.1016/j.freeradbiomed.2012.08.590.
