Day 2 :
Keynote Forum
Roland Hetzer
Medical Director of Herzzentrum Cottbus
Keynote: Progress in the treatment of end-stage heart failure
Time : 09:00-09:40

Biography:
Prof. Dr. Roland Hetzer has completed his cardiothoracic surgery training in Hannover Medical School, Germany and in Stanford University, California. He performed the first heart transplantation in Hannover in 1983 and the first pediatric heart transplantation in Germany in 1985. As the Medical Director and Chairman in Deutsches Herzzentrum Berlin from January 1986 to September 2014, he and his team performed more than 1900 heart transplantations and more than 2300 implantations of mechanical circulatory support systems. He has made numerous original contributions in the field of cardiothoracic and vascular surgery particularly in surgical treatment of end-stage heart failure and valve surgery. Presently, he still serves as the Medical Director of Herzzentrum Cottbus and sees his private patients in Cardio Centrum Berlin.
Abstract:
Heart failure has a rapidly increasing incidence in both men and women and is the most prominent heart disease in the elderly. This is due to the successful treatment of acute heart disease which later on turns into chronic failure. Whereas pharmaceutical and electrophysiological concepts have been constantly improved, end-stage heart failure has been approached by various surgical procedures.
The majority of cases depends on ischemic heart disease which we described as LOCIMAN (Left heart failure, Occlusion of the Coronary artery, Incompetence of Mitral valve and Left ventricular Aneurysm or Akinesia). It appears to be mandatory to evaluate the relative contribution of these components to heart failure and the relative importance of surgical procedures (coronary bypass, mitral valve repair and aneurysmectomy) for cardiac improvement.
These procedures play a major role in less than profound heart failure. In such cases, various external support procedures were introduced which mostly have been abandoned as well as the partial ventricular resection procedure (Batista).
Neither external restraint procedures have not fulfilled the expectations nor myocardial regeneration and stem cell application.
Heart transplantation is now a well-established treatment for end-stage heart failure, enabling a high degree of physical rehabilitation and a mean survival time of 12 to 14 years. Some of our patients are now living for more than 30 years after transplantation. However, heart transplantation is an option offered to only few patients due to limited availability of donor organs.
Mechanical circulatory support systems have achieved clinical application during the last 30 years. Between 1987 and 2014, more than 2300 ventricular assist devices have been implanted in Berlin to keep patients alive, after which there were three options: bridge to transplantation, bridge to myocardial recovery in myocarditis and in cardiomyopathy, first demonstrated by pump explantation and long-term stability in Berlin in 1995, and as permanent implants.
Originally these ventricular assist devices were extracoporeal connected to large driving units. Thereafter, electrical pulsatile systems were introduced; however, these were noisy and bulky. In 1998, the author implanted the first rotary blood pump with continuous flow (MicroMed DeBakey) worldwide. Such systems, which are small and silent, have become the standard in now 90% of cases. These pumps also qualify for long-term use (up to 10 years). They are developed to support the left ventricle; however, they can be also implanted in the right ventricle when necessary. Moreover these systems are very useful in elderly patients.
Pulsatile extracorporeal systems, i.e. Berlin Heart EXCOR Pediatric, are the only one available for end-stage heart failure in infants and young children.
Complete myocardial recovery has been observed with ventricular assist device support in acute myocarditis and even in dilative cardiomyopathy.
The only available total artificial heart is the CardioWest pneumatic system. However, there are some experimental total artificial heart developmental projects going on in Germany, in France and in USA.
Keynote Forum
Robert Skalik
Wrocław Medical University, Poland
Keynote: Adaptive physiology or cardiovascular dysfunction - how to optimize diagnostic management in athletes?
Time : 09:30-10:20

Biography:
Robert Skalik is a Consultant in Cardiology at two hospitals (Regional General Hospital, Krotoszyn and Leszno Medical Centre “Ventriculus”, Leszno, Poland) and outpatient Cardiology Clinics in WrocÅ‚aw. He is an academic Teacher in Department of Physiology, Medical University of WrocÅ‚aw, Poland, former Consultant in Cardiology and Echocardiography, Department of Cardiac Surgery and Cardiology, Medical University of WrocÅ‚aw. He completed his PhD in Echocardiography at Medical University of WrocÅ‚aw, Poland. He completed his internship in Department of Cardiology, Free University of Amsterdam, Netherlands. He was a Lecturer at Post-graduate School of Cardiology, University of Perugia, Italy. He is a member of editorial and review boards for medical journals: Clinical and Medical Investigations, Journal of Cardiovascular Disorders, SRL Cardiology, Annals of Cardiology and Cardiovascular Diseases, Reviewer of International Journal of Cardiology, Expert Review of Cardiovascular Therapy, Reviewer of research projects on Cardiovascular Medicine and Physiology co-funded by European Commission, Author of 107 published reports.
Abstract:
Athletic training presents a burden on the cardiovascular system and can pose a significant risk in athletes with undetected heart anomaly. Asymptomatic or symptomatic heart abnormality in athletes usually includes ventricular systolic or diastolic dysfunction caused by myocarditis, ischaemia, and hypertensive, hypertrophic or dilated cardiomyopathy. Nonetheless, other cardiac pathologies such as congenital or acquired heart dysfunction and valve defects can also contribute to cardiovascular fatalities in athletes. A growing interest in sports activities raises concerns regarding the safety of exercise in athletes with various cardiovascular anomalies. In recreational sports, the incidence of sudden cardiac death and cardiovascular comorbidities is higher than expected and may even increase as more and older individuals participate in organized sports. The risk of unrecognized symptomatic or asymptomatic left ventricle remodeling with subsequent heart dysfunction or heart failure in athletes increases with age. Moreover, a greater number of patients with a history of cancer treated with cardiotoxic therapy seek participation in sports. Equipped with an improved diagnostic and treatment armamentarium, and faced with a growing number of “at risks” participants, sports cardiologists will be increasingly faced with the dilemma of qualifying this population for exercise. The various aspects of cardiac hypertrophy, their relevance for understanding the differential diagnostic process, pathophysiologic mechanisms of cardiovascular dysfunction in athletes and whole array of diagnostic tools used in the specific group including ECG, cardiopulmonary exercise testing and advanced imaging techniques are discussed.
References:
- Robert Skalik. Screening of athletes : an electrocardiogram is not enough Herz 2015
- Robert Skalik. Qualifying athletes for exercisee-J.Cardiol.Pract. 2014
- Robert Skalik, Branko Furst. Heart failure in athletes: pathophysiology and diagnostic management. e-Journal of Cardiol.Pract. 2017
- Robert Skalik, Anna Janocha, LudmiÅ‚a Borodulin-Nadzieja, Anna Goździk, RafaÅ‚ PorÄ™ba, Dariusz BiaÅ‚y, Arkadiusz Derkacz, Marta Obremska, Ireneusz CaÅ‚kosiÅ„ski. The effect of different exercise protocols on leptin levels and regional left ventricular diastolic heart function among professional swimmers - a comparison with untrained subjects: a Doppler tissue imaging study Med.Sport.(Kraków) 2006
- Dariusz Biały, Arkadiusz Derkacz, Halina Nowosad, Robert Skalik, Edyta Marszałek, Rafał Poręba, Marcin Protasiewicz, Zdzisław Zagrobelny. Electrocardiography and echocardiography in athletic heart imaging, Biol.Sport. 2003
- Cardiac Surgery | Heart Failure | Myocardial Infarction | Sports Cardiology | Cardio-Oncology | Case Reports on Cardiology
Location: Amphi Theatre

Chair
Aris Lacis
Children Clinical University Hospital, Latvia

Co-Chair
Marco Piciche
San Camillo-Forlanini Hospital, Italy
Session Introduction
William E Feeman Jr.
Wood County Hospital, USA
Title: Statin therapy in a 101 year old survivor of myocardial infarction
Time : 10:20-10:45

Biography:
William E Feeman is a Physician at Wood County Hospital. He is the Founder of Association for the Prevention of Atherothrombotic Disease in Northwest Ohio to facilitate the spread of knowledge about this disease.
Abstract:
There is not a consensus of opinion on statin therapy of dyslipidemia in the oldest of the very of patient population. This is a case report of a 75 year old woman who sustained an acute myocardial infarction. Because her attending physician did nothing in the way of treating her dyslipidemia, the patient began to attend the author’s clinic. She started to take stain therapy and aspirin. Her initial course was marked by recurrent chest pains, and a calcium channel blocker was added. The chest pains subsequently resolved and the patient has done well on super-stain therapy, combined with aspirin and calcium channel therapy—with no other interventions, medical or surgical. She is doing well, living in her own home, at age 101½ years. This is a report of a unique case showing that optimal medical therapy including super-stain therapy can be effective in controlling dyslipidemia even in the oldest of the very old patients with dyslipidemia.
Reda Biomy Mohamed
Benha University, Egypt
Title: Effect of chronic hepatitis C virus treatment by combination therapy on cardiovascular system
Time : 11:00-11:25

Biography:
Reda Biomy completed his Graduation at Benha University, Egypt and MD in Cardiology 1992. In 1995, he worked as an Associate Professor of Cardiology at Benha University, Egypt and he was responsible for non-invasive cardiology lab and cardiac catheterization lab.
Abstract:
Introduction: The prevalence of hepatitis C virus (HCV) in Egypt is quite high and the recent introduction of combined oral direct antiviral agents may have impressive results.
Aim: Aim of this study is to assess the cardiovascular effects of direct acting antiviral agents (DAAs) in combination with or without pegylated interferon alpha (PEG-IFN) in Egyptian patients with chronic hepatitis C infection.
Methods: This study included 170 patients suffering from chronic hepatitis C virus infection. Patients were divided into two groups; first group (100 patients) received triple combination therapy in the form of pegylated interferon alpha, sofosbuvir (sovaldi) and ribavirin, while second group (70 patients) received dual combination therapy in the form of sofosbuvir and simeprevir (sovaldi and olysio). Group one patients were followed up for one year over three visits; before initiating treatment, then six months and 12 months later while group two patients were followed up for six months over two visits; before initiating treatment and then six months later and the end point of the study was either development of a major cardiovascular event throughout the course of the study (e.g. congestive heart failure, echocardiographic evidence of LV dysfunction, occurrence of significant arrhythmias or acute coronary syndrome) or completing till the end of the study without any evidence of cardiac affection. The following parameters were accomplished, thorough medical history and clinical examination, ECG, echo-Doppler study and laboratory investigations.
Results: No significant differences were found between the two study groups as regards demographic criteria. None of both group patients had developed any major cardiac event (e.g. congestive heart failure, echocardiographic evidence of LV dysfunction, occurrence of significant arrhythmias or acute coronary syndrome). No significant changes as regards ST-T wave abnormalities or arrhythmias had occurred six and twelve months after initiation of treatment compared to baseline visit. None had developed prolonged QT interval at follow up visit. No significant changes were seen in the mean values of corrected QT in group two patients over study visits (p value>0.05). None of both group patients had or developed echocardiographic regional wall motion abnormalities (RWMA) at baseline or at study end. Systolic function parameters showed minute non-significant changes over study visits (p value>0.05). Diastolic function parameters (E/A ratio, deceleration time and E/Ea ratio) showed non-significant changes between baseline and 6- and 12 month visits (p value>0.05).
Conclusion: The direct antiviral agents used in combination regimen with interferon (pegylated interferon alpha, sofosbuvir and ribavirin) or used orally in combination (sofosbuvir and simeprevir) not significantly affect the cardiovascular system.
Aris Lacis
Children Clinical University Hospital, Latvia
Title: Using stem cells for stimulating tissue regeneration and functional activity in a wide spectrum of pathologies
Time : 11:25-11:50

Biography:
Aris Lacis is a Cardiac Surgeon and Professor. He completed his Graduation at Riga Medical Institute in 1961. He was a General and Thoracic Surgeon at P. Stradins University Hospital in Riga (1964–1969); Thoracic and Cardiac Surgeon at Latvian Centre for Cardiovascular Surgery (1969–1994) and; Head of Pediatric Cardiology and Cardiac Surgery Clinic at University Children’s Hospital, Riga (1994-2012). He is the President of Latvian Association for Pediatric Cardiologists, Author of 395 scientific publications, three monographs and 13 patents. He is an Investigator of more than 10 clinical trials including Cardio-surgical procedures performed under deep hypothermia and hybrid procedures etc.
Abstract:
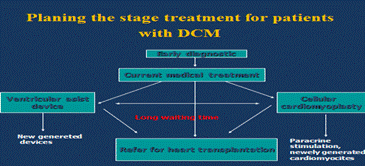
Statement of the Problem: Dilated cardiomyopathy is a serious problem in pediatric cardiology praxis. Despite the relatively low incidence of 0.57 to 2.6 per 100000 children, the mortality rate is high. One third of patients die within the first year after diagnosis. Up to 40% of these patients are defined as idiopathic dilated cardiomyopathy (IDCM), characterized by ventricular dilation and systolic dysfunction. Researchers have reposted that conventional medical therapy does not improve the outcome of the disease; however, recent clinical studies have suggested bone marrow derived autologous mononuclear cells as a promising therapy option. Pulmonary arterial hypertension (PAH) is characterized by increased pulmonary vascular resistance resulting in extensive heart structural changes leading to right heart failure and death. PAH is characterized by obstruction of small pulmonary arteries leading progressive increase in vascular resistance. Locally implanted stem cells may trigger the neovascularization process in the lung potentially leading to a decrease of pulmonary artery pressure.
Methodology: For treatment of IDCM, we prefer to use transcutaneous intramyocardial administration of autologous bone marrow derived mononuclear stem cells, combined with ultrasound monitoring. In patients with PAH intrapulmonary transplantation of stem cells was performed using intravasal injection of the stem cells by catheterization pulmonary arteries and directly in the lung tissues by using standard thoracentesis technique, performed under chest radiological control.
Conclusions: If applied wisely, the stem cell therapy appears to be a safe and effective way for stabilization of critically ill patients with both severe pulmonary arterial hypertension and idiopathic dilated cardiomyopathy. This method provides additional opportunities for symptomatic treatment and serves as a bridge for potential heart and lung transplantation.
References:
1. “Intramyocardial administration of autologous bone marrow mononuclear cells in a critically ill child with dilated cardiomyopathy”. LÄcis A., Ä’rglis A. Cardiology in the Young, 2011, 21, 110–112
2. “Neo-revascularization as the potential treatment for patientsuffering from pulmonary hypertension (Myth or reality?)” LÄcis A., Lubaua I., Ä’rglis A. et al. J. Clinical Medicine Research (CMR), 2013, 2 (3): 32–36
3. “Management of idiopathic dilated cardiomyopathy with intramyocardial cell transplantation in children. A retrospective study of 7 patients” LÄcis A., Lubaua I., Ä’rglis A. et al. J. Clinical Medicine Research (CMR), 2013, 2 (4): 129–133
4. “Safeguards and pitfalls in technique used for stem cell delivery in children suffering from idiopathic dilated cardiomyopathy” LÄcis A., Lubaua I., Ä’rglis A. et al. Journal of US-China Med. Science, 2013, vol. 10, N 3–4, 71–75
5. “Stem cell therapy as one of temporary measures for management of heart failure and pulmonary hypertension in children” LÄcis A., Lubaua I., Ä’rglis A. et al. American Journal of Experimental and Clinical Research, 2014, 1 (3): 38–46
Marco Piciche
San Camillo-Forlanini Hospital, Italy
Title: The nature and enigma of the noncoronary collateral circulation
Time : 11:50-12:15

Biography:
Marco Piciche completed his Graduation in Medicine at University of Florence in 1995 and Cardiac Surgery Residency at Tor Vergata University of Rome in 2000. He has worked as an Assistant at Saint Luc Hospital, Catholic University of Louvain, Brussels (1999–2001), as a Clinic Head/Hospital Assistant at universities of Clermont-Ferrand (2003–2004) and Montpellier (2004–2007). In Canada, he authored a research project on ‘‘Noncoronary collateral circulation,’’ which was submitted to the annual research competition at Québec Heart & Lung Institute, Laval University, and received the competition’s highest grant. In September 2011, he completed his PhD in Therapeutic Innovations from Paris-Sud University. He is the Editor in Chief of the book Dawn and Evolution of Cardiac Procedures-Research Avenues in Cardiac Surgery and Interventional Cardiology. Currently, he is a Consultant Cardiac Surgeon in Italy.
Abstract:
Notwithstanding the fact that the coronary collateral circulation (CCC) is the only blood supply warranting ongoing attention, the human heart benefits from a small additional source of blood, called noncoronary collateral myocardial blood flow (NCCMBF) or noncoronary collateral circulation (NCCC). It consists of a small blood supply reaching the heart through a micro-vascular network arising from the bronchial, esophageal, pericardial and diaphragmatic arteries. These small channels enter the heart through the pericardial reflections surrounding the pulmonary and systemic veins, connecting with the vasa vasorum of the aorta and pulmonary artery. The left and right internal mammary arteries (ITAs), along with their collateral branches, are among these non-coronary sources. Under certain circumstances the ITAs have a high potential for developing collateral branches. In the case of severe Leriche syndrome or with chronic obstruction of the abdominal aorta, the ITAs can serve as the main or even sole source of blood supply to the lower limbs. Communication is also possible between the ITAs and the native coronary arteries. This has been demonstrated by angiography in living patients, both for right and left coronary artery disease. Postmortem angiography in patients with ischemic heart disease has demonstrated such connections in 12% of cadavers. The Vineberg operation of the 1940s was based on the plastic potential of the ITAs. It consisted of ITA implantation into the left ventricular wall, with development of an extensive collateral network visible at angiography even at very long-term follow-up. It has been recently demonstrated that in ischemic conditions there is a functional, ischemia-reducing extracardiac coronary artery supply via natural ipsilateral ITA anastomosis. Herein, the available data on the non-coronary blood supply to the human heart have been reviewed.
References:
- Picichè M. Noncoronary Collateral Myocardial Blood Flow: The Human Heart’sForgotten Blood Supply. The Open Cardiovascular Medicine Journal, 2015, 9, 105-113
- Picichè M, Kingma JG, Voisine P, Dagenais F, Fadel E. Angiogenesis and surgical or endovascular enhancement of noncoronary collateral circulation: A new research field. J Thorac Cardiovasc Surg 2010; 139 (6): 1675-6.
- Picichè M, Kingma JJ, Fadel E, Dagenais F, Mathieu P , Simard D, De Maria RG, Voisine P. Enhancement of noncoronary collateral blood flow from the internal thoracic arteries: the theoretical and practical basis of an alternative method of myocardial blood supply. J Cardiovasc Surg 2011; 52(1):127-31
Rachad M Shoucri
Royal Military College of Canada, Canada
Title: A look at heart failure based on the study of end-systolic pressure-volume relation (ESPVR)
Time : 12:15-12:40

Biography:
Rachad M Shoucri completed his BSc in Electrical Engineering at Alexandria University, Egypt; MSc in Optical Physics and; PhD in Theoretical Physics at Laval University, Québec, Canada. After graduation in 1975, he worked for five years at the Hôpital Saint-Sacrement and the Institut de Cardiologie de Québec where he developed his current interest in Mathematical Physiology and in the application of mathematics in cardiology. Since 1981, he is working in Department of Mathematics and Computer Science at Royal Military College of Canada, Kingston, Ontario.
Abstract:
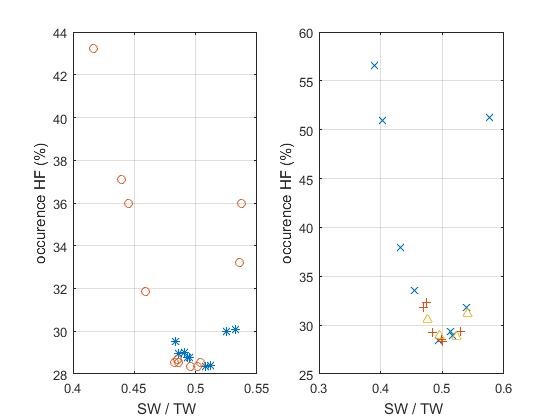
Parameters describing the linear and non-linear models of the end-systolic pressure-volume relation (ESPVR) in the heart ventricles have been derived, relations of these parameters with the ejection fraction (EF) have been obtained. The relations between the parameters of the ESPVR and EF can be applied to the study of the problem of heart failure with reduced or preserved EF (HFpEF). The results of this study show that important information concerning the problem of HFpEF can be derived from the parameters describing the ESPVR. Applications to clinical data published in the literature show the consistency of the mathematical formalism used to calculate the equation of the non-linear ESPVR in which formalism is based on the theory of large elastic deformation of the myocardium. The results presented in the figures show one possible application, the relation between the percentage occurrence of heart failure (HF) and the ratio SW/TW (SW=stroke work, TW=total area under the ESPVR). The results are presented on two figures for the purpose of clarity for five clinical groups: normal*, aortic stenosis o, aortic valvular regurgitation +, mitral regurgitation ^, miscellaneous cardiomyopathies x. Note that both curves have a minimum around SW/TW≈0.5. Note also that the normal group (*) appears near the minimum of the curve on the left hand side (corresponding to EF≈0.67). The case of aortic stenosis on the left hand side appears in three subgroups. Calculation indicates an optimal value of SW/SWx≈0.8 (SW=stroke work, SWx=maximum stroke work corresponding to a given ESPVR). The quantity SWR=SWx–SW is the stroke work reserve; we have calculated SWR/SW≈0.25 for SW/TW≈0.5.
References:
- Dumesnil JG, Shoucri RM, Laurenceau JL, Turcot J (1979) A mathematical model of the dynamic geometry of the intact left ventricle and its application to clinical data. Circulation 59: 1024-1034
- Shoucri RM (2010) ESPVR, ejection fraction and heart failure. Cardiovasc. Eng. 10: 207-210.
- Shoucri RM (2015) End-Systolic Pressure-Volume Relation, Ejection Fraction, and Heart Failure: Theoretical Aspect and Clinical Applications. Clinical Medicine Insights: Cardiology 9(S1): 111-120.
- Da Mota JPGF (2013) Intelligent modeling to predict ejection fraction from echocardiographic reports. MSc thesis in Mech Eng, IST Técnico Lisboa, Portugal.
- Curtis JP, Sokol SI, Wang Y, Rathore SS, Ko DT, et al (2003) The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J Am Coll Cardiol 42 (3): 736-742.
Fabiola B Sozzi
University Hospital Policlinico of Milan, Italy
Title: Congenital coronary fistulae: Clinical impact and interesting cases
Time : 12:40-13:05

Biography:
Fabiola B Sozzi works as a Staff Cardiologist at University Hospital Policlinico of Milan, Italy. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She has expertise in Echocardiography at Thoraxcenter of Rotterdam (NL), where she defended her PhD thesis on Stress Cardiac Imaging under the supervision of Professor J Roelandt. She is a Visiting Professor at University of Milan where she leads several research projects and teaches at Faculty of Medicine and School of Specialization of Cardiology. She is an Author of 70 papers published in peer-reviewed international journals and Reviewer of several medical international journals.
Abstract:
Coronary fistulae (CAF) with the cardiac chambers are extremely rare congenital vascular anomalies, reported in approximately 0.08-0.3% of unselected patients. Although coronary artery fistulae are commonly asymptomatic, they may cause severe symptoms depending on the severity of the shunt. Little data on the clinical impact and treatment are available. We aim to determine the outcome of percutaneous closure of large hemodynamically significant CAF in young patients. We retrospectively analysed 11 patients (median age at intervention 21 years, three females) affected by relevant congenital CAF, diagnosed by echocardiogram and cardiac catheterization. All patients underwent percutaneous closure and were followed for a mean period of three years. The clinical presentation of CAF was characterized by symptoms. In some cases CAF was incidentally diagnosed by echocardiogram. Most fistulas were originating from the left coronary artery (LCA) [7/11]. The right heart was the most common site of drainage (8/11). Multiple fistulas were found in three patients. No-one had other congenital disorders associated. All patients were treated with percutaneous transcatheter embolization. During follow-up, no patient died. In one case a retrograde thrombosis of the fistula with acute myocardial infarction occurred after one month and was treated with thrombectomy and coronary bypass. No other major adverse cardiac events were recorded. We conclude that the percutaneous closure of significant CAF is associated with low event-rate and excellent prognosis. A rich iconography based on echocardiography, computed tomography, magnetic resonance imaging and angiography are presented for some interesting cases.
- Workshop on: "Torsades de Pointes (TdP)"
Location: Amphi Theatre
Session Introduction
Guy Hugues Fontaine
Universite Pierre et Marie Curie & La Salpetriere Hospital, France
Title: Torsades de Pointes (TdP)
Time : 14:05-15:05

Biography:
Guy Hugues Fontaine has made 16 original contributions in the design and the use of the first cardiac pacemakers in the early 60s. He has serendipitously identified ARVD during his contributions to antiarrhythmic surgery in the early 70s. He has developed the technique of fulguration to replace surgery in the early 80s. He has been one of the “216 individuals who have made a significant contribution to the study of cardiovascular disease since the 14th century”, one of the “500 greatest geniuses of the 21th century” (USA Books), one of the “100 life time of achievement” (UK Book). He has 900+ publications including 201 book chapters. He is a Reviewer of 21 scientific journals both in basic and clinical science. He has developed new techniques of hypothermia for neurologic brain protection in OHCA, stroke and spinal cord injury. He has also recently invented a high-tech device which can be considered as the ultimate in palliative care.
Abstract:
Torsades de Pointes (TdP) is a rare but important cause of sudden death of young people with the genetically determined long or short QT syndrome. The length of the QT interval is directly related to the risk stratification of these patients modulated by genetic factors. TdP is also a major concern of the pharmaceutical industry for the development of any cardiac and even non-cardiac drugs. Endocardial recordings during TdP in human have brought new concepts for the understanding of this arrhythmia mechanism. Here, presence of intramyocardial conduction defects is demonstrated by the analysis of endocardial potentials observed on the QRS complexes in complete AV block. We present for the first time that patients (old females) with spontaneous complete AV block have a trouble in conduction not only on the AV conduction system but also inside the myocardium. This concept is reinforced by the absence of EGM but only far field potentials observed several times presented in a unique case. These images document the concept of depressed myocardium in which not only AV conduction but also intramyocardial conduction is impaired. It may explain that most TdP are transient and return spontaneously to sinus rhythm. Other data have demonstrated the presence of Wenckebach type I and Mobitz type2 in the myocardium of those patients suggesting that the myocardium has preferential pathways working as conduits transmitting ventricular activation. This is also in agreement with the identification of a specific genetic background.
- Heart Failure | Myocardial Infarction | Cardiac Surgery | Sports Cardiology | Cardio-Oncology | Case Reports on Cardiology
Location: Amphi Theatre

Chair
Aris Lacis
Children Clinical University Hospital, Latvia

Co-Chair
Marco Piciche
San Camillo-Forlanini Hospital, Italy
Session Introduction
Jean-Pierre Usdin
American Hospital of Paris, France
Title: Cardio-oncology, a medical speciality for these linked pathologies
Time : 15:05-15:30

Biography:
Jean-Pierre Usdin is a former Internal of the Hospitals of Paris, former Head of clinic, Assistant of hospitals of Paris, former Consultant of scientific committee of medical journal Consensus and previous Chief of the Cardiologic department of American Hospital of Paris (2006-2012). He is currently renowned Cardiologist at American Hospital of Paris, member of European Society of Cardiology and member of French Society of Cardiology. Being a Journalist and Blogger in Medscape France from 2010, he has blogs dedicated to general cardiology: Reports discussions and notes about trials, cardiology congresses, live-comments on 2015 ESC Congress in London.
Abstract:
Cardiovascular diseases and cancer are the leading causes of death from non-communicable diseases in the world. These two top killers share not only this characteristic but have common specificities. Risk factors are some modifiable: Tobacco, social custom sedentarity, environment, others are not: Age, heredity. Cardiovascular health cancer therapies occupy an important place. As cancer therapies are more and more active, affected people are cured or living longer, so heart disease is an emerging problem in this population. For this purpose a sub speciality: Cardio-oncology was created. Cardio oncology permits specialists of cardiology and oncology not only to share the immediate but the long term of illnesses. As example, in the past, we all know the effects of chemotherapy (anthracyclines) on myocardial function, the occurrence of constrictive pericarditis many years after chest radiotherapy. But new cancer treatments like immunotherapy, hormonotherapy, cell specific inhibitor antibodies, are no safer and interfere with heart and vascular function. According to my knowledge, there is no cardiologist regularly invited in multidisciplinary staff meetings, debating pros and cons of patient’s treatments. On the other side, cardiac therapies are sometimes pointed out to provoke (statin) or protect from (aspirin) cancer when prescribed on a long term basis. Cardio oncology speciality will permit in the very next future to unify in one specialist the treatment of these frequently associated pathologies.
Syed M S Mujtaba
Freeman Hospital, UK
Title: Extended trans-septal versus left atrial approach in mitral valve surgery: 1017 patients experience
Time : 15:30-15:55

Biography:
Syed M S Mujtaba completed his Graduation at Dow Medical College, Karachi, Pakistan in 1985. He did his basic and higher Surgical training in Ireland and FRCS in 1993. He started Cardiothoracic Surgery at University Hospital Cork, Ireland in 1994. In 1997, he started his training in Cardiothoracic Surgery at Yorkshire Heart Centre, Leeds, UK. He worked for two years in Dubai as Senior Registrar. He joined as Consultant Cardiac Surgeon at Liaquat National Hospital, Karachi, Pakistan and worked for three years. Then, he worked as Consultant in Tabuk, Saudi Arabia for 18 months and as Medical Director at Baqai Centre for Cardiovascular diseases, Karachi for a year.
Abstract:
Statement of the Problem: The mitral valve may be accessed directly through the left atrium but visualization can sometimes be challenging. A trans-septal inter-atrial approach provides better exposure and easy access for concomitant tricuspid procedures especially in difficult cases. This retrospective study evaluates the safety and effectiveness of the extended vertical trans-septal approach for routine mitral valve exposure.
Methodology & Theoretical Orientation: 1017 consecutive patients undergoing an isolated primary mitral valve procedure (repair/replacement) through a median sternotomy were retrospectively studied between 2000 and 2015. 135 patients were operated by extended vertical trans-septal approach (EVTSA, group A) while 882 patients underwent a traditional left atrial (LA, group B) approach.
Findings: There were 135 patients (M/F=56/79) in group A and 882 patients (M/F=398/484) in group B. Logistic EuroSCORE was significantly lower in EVTSA group (0.61 vs. 0.90 p=0.000001). In the LA group, there were more patients with pre-operative TIA or stroke (94 vs. 6, p=0.005). Cumulative cross clamp time was 82 (44-212) minutes (EVTSA) and 78 (30-360) minutes (LA) groups (p=0.271) while cardiopulmonary bypass time was 107 (58-290) and 114 (43-602) minutes respectively (p=0.121). Post-operative blood loss was 415 ml (EVTSA) versus 427(LA) ml (p=0.273). No significant difference was found in the incidence of post-operative atrial fibrillation (p=0.22) or heart block requiring permanent pacemaker (p=0.14).
Conclusion & Significance: An extended vertical trans-septal approach to the mitral valve is safe and reproducible. It gives excellent exposure of the mitral valve under all circumstances without any significant increase in cross clamp or bypass time, post-operative arrhythmia, heart block/pacemaker rate or bleeding.
Porawan Bunleng
Bumrungrad International Hospital, Thailand
Title: Strategies for improving door-to-ECG time in acute coronary syndrome patients: Bumrungrad International Hospital
Time : 16:10-16:35

Biography:
Porawan Bunleng completed her Graduation at Faculty of Nursing, Khon Kaen University. She has 15 years of experience in Nursing and eight years of experience at Heart Center, Bumrungrad International Hospital. She has an experience of Supervising and Overseeing the Nursing department to meet the specified goals; controlling service standards; administering the organizational and personnel works and managing the medical supplies to meet the policy; reviewing administrative process and procedures to achieve efficient results.
Abstract:
Background: Target ACS is a hospital quality initiative by setting challenging target for achieving the door-to-ECG time goal of 8 min ACS patients (The goal standard of door-to-ECG time benchmark is <10 min). Our hospital’s STEMI sub-committee recognized the importance of improving door-to-ECG times due to the benefit of a rapid initial ECG results can lead to rapid reperfusion.
Aim: Aim of this study is to improve door-to-ECG time for achieving door-to-ECG time goal of 8 min in ACS patients.
Methods: This study was conducted at the Bumrungrad International Hospital, Thailand. This hospital has 580 in-hospital beds and emergency cardiac catheterization is available 24 hours. Multi-component strategies includes: Provide infrastructure in an especially high-risk area for heart attack in hospital to facilitate early identification of critical arrhythmias such as ECG monitoring, fast track communication, etc.; develop a standardized annual education program to ensure ongoing competency in ECG acquisition skill to identify STEMI patients in the field; having a dedicated quality assurance process to monitor performance of the STEMI bypass system, and; a real time dashboard to monitor STEMI performance and using for gap analysis based on a comparison of current practice and best practice to development of consensus recommendations for improvements in the management of STEMI patients in hospital.
Results: A total of 257 patients included in the study: 112 before (January to December 2014) and 145 after intervention (January to December 2016). Before the intervention, 48% received an ECG at 8 min or less. After the intervention, 97% met the time requirement, for a mean difference of 49%. The mean (min-max) time from door-to-ECG was decreased by 4 min after the intervention.
Conclusions: The overall percentage of patients with a door-to-ECG time within 8 min improved without increasing staffing.
Maja Karaman Ilic
General Hospital Sveti Duh & Josip Juraj Strossmayer University of Osijek, Croatia
Title: Non-invasive postoperative extravascular lung water monitoring
Time : 16:35-17:00

Biography:
Maja Karaman Ilic is an Anesthesiologist subspecialized in Intensive Care. She is dealing with perioperative fluid management for an extensive period of time. She has completed PhD in the field of Anesthesiology. She is experienced in using ultrasound in a diagnostic and therapeutic way for critical care patients.
Abstract:
Statement of the Problem: Pulmonary complications that occur after major thoracic and abdominal surgical procedures are the primary reason for extending a patient's stay in the intensive care unit. Complications range from atelectasis and pulmonary edema to pneumonia, acute lung injury and acute respiratory distress syndrome. Fluid replacement therapy is unavoidable during surgery. Too much fluid can cause rise in extravascular lung water (EVLW) and result with pulmonary edema. Assessment and monitoring of EVLW traditionally has relied upon invasive computed tomography (CT) or pulse counter cardiac output (PiCCO) testing. A less invasive and accurate alternative is the PaO2 to FiO2 (P/F ratio). A potentially sensitive non-invasive procedure for EVLW rise detection during early postoperative period is lung ultrasound.
Methodology & Theoretical Orientation: Since ultrasound waves are completely reflected by air, they can image the parenchyma only when interstitial-alveolar imbibition occurs. This gives rise to characteristic vertical artifacts called “B-lines”. The number of B-lines is directly proportional to the degree of lung aeration loss and to EVLW volume.
Findings: In our study, by use of lung ultrasound, volume small enough to produce shunting of ≤20% was detected before other clinical signs of EVLW rise.
Conclusion: Using lung ultrasound B-lines to detect EVLW has not been tested extensively, and it has not been compared with the conventional index of P/F ratio. If it allows accurate EVLW assessment, lung ultrasonography could become very useful tool in early detection and prevention postoperative pulmonary edema due to intraoperative fluid overload.
Syed M S Mujtaba
Freeman Hospital, UK
Title: Early clinical results of perceval suture-less aortic valve in 139 patients: Freeman experience
Time : 17:00-17:25

Biography:
Syed Saleem Mujtaba completed his graduation at Dow Medical College, Karachi, Pakistan in 1985 and; basic and higher Surgical training in Ireland and FRCS in 1993. He started Cardiothoracic Surgery at University Hospital Cork, Ireland in 1994. In 1997, he started his training in Cardiothoracic Surgery at Yorkshire Heart Centre, Leeds, UK. He worked for two years in Dubai as Senior Registrar. He was a Consultant Cardiac Surgeon at Liaquat National Hospital, Karachi, Pakistan and worked for three years. Then, he worked as Medical Director at Baqai Centre for Cardiovascular diseases, Karachi for a year. He worked as Clinical Fellow in Cardiothoracic Surgery for 18 months at Edinburgh Royal Infirmary in 2011. He moved to Freeman Hospital, Newcastle UK in March 2013 as Clinical Fellow and still working there. He completed his FRCS (CTh) in 2016.
Abstract:
Statement of the Problem: The aim of this retrospective study is to evaluate the safety and performance of the perceval suture-less valve in patients undergoing aortic valve replacement (AVR). We report the 30-day clinical, echocardiographic and hemodynamic outcomes of 139 patients.
Methodology & Theoretical Orientation: From January 2014 to December 2026, 139 patients underwent suture-less aortic valve replacement. Their operation notes, PACS records and per operative TOE findings were studied retrospectively. Patients with bicuspid aortic valve and abnormal STJ: annulus ratio was excluded.
Findings: 92 patients underwent isolated aortic valve replacement (group A) with perceval valve and 47 patients had combined procedures of AVR and coronary artery bypass grafting (group B). The patients received a size S (n=23), M (n=39), L (n=42) or XL (n=35) prosthesis. Perceval valve was successfully implanted in 135 patients (97.1%). Mean cross clamp and bypass time was 40 and 63 minutes for isolated cases, while it was 68 and 107 minutes for combined cases. Three patients (2.1%) died within 30 days. Four patients suffered stroke and five patients went into acute renal failure. Median ICU and hospital stay was 2 and 8.5 respectively. Four valves were explanted due to significant para-valvular leak after surgery. Five patients had permanent pacemaker as a result of complete heart block and mean post-operative drainage was 295 ml for isolated case and 457 ml for combined cases.
Conclusion & Significance: Early post-operative results showed that perceval valve is safe. It can be implanted with short cross clamp and bypass time. Further follow up is needed to evaluate the long-term outcome with this bio-prosthesis.
